
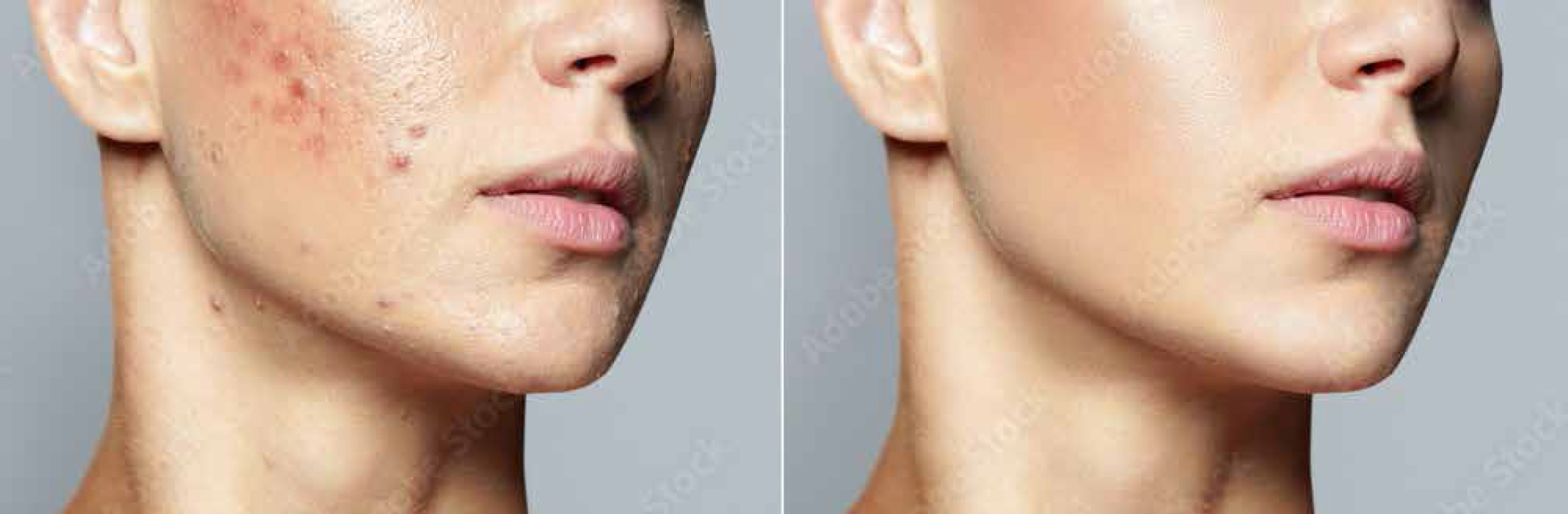
Guidelines of care for the management of acne vulgaris
Acne vulgaris is a common skin condition that affects preadolescents from the age of nine, adolescents and adults. The aim of this study was to look at the research and to recommend evidence-based treatments for acne. To perform this study, the authors carried out a systematic review. There was a total of 18 evidence-based recommendations with 5 recommendations that were deemed to be excellent. The most commonly made recommendations for acne treatment were benzoyl peroxide, topical retinoids, topical antibiotics and oral doxycycline. Oral isotretinoin is also recommended for acne but this is strongly recommended for severe acne. This, however, can cause psychosocial burden and is also recommended to treat scarring, or for those for whom oral or topical therapy was not successful. Other recommendations that were made were topical clascoterone, salicylic acid, and azelaic acid. Oral minocycline, sarecycline, the combined oral contraceptive pills, and spironolactone were also recommended. It was also suggested to use a combination of topical therapies with multiple mechanisms of action, which would limit antibiotic use. For larger acne lesions, it was recommended to add corticosteroid injection. All recommendations from the authors were based on the available evidence at the time of the systematic review. The authors have suggested that these guidelines will help to provide clinicians with evidence-based recommendations for the management of acne vulgaris.
A survey on the cosmetic use of injectable polynucleotide: the pattern of practice among Korean dermatologists
Skin boosters are a hugely popular treatment, used worldwide to help improve the skin in regards to the texture, elasticity, hydration and overall appearance of the skin. Polynucleotides have recently become very popular, but there is still very little information regarding their use. The aim of this study is to research this popular treatment and to evaluate the safety and efficacy of polynucleotides. For this study, a total of 235 Korean board-certified dermatologists took part in a survey. All of them had experience of using skin boosters. This survey had questions relating to the dermatologists practice, how they chose their product and what other devices they had in their clinic. For the dermatologists that already use polynucleotides in practice, they were asked to check the clinical indications, mode of delivery, injection depth, treatment interval, as well as options for combined therapy in relation to the polynucleotides. The results of the study showed that 71% of the dermatologists had at least 5 years' experience as a board-certified dermatologist, and among the different skin boosters available to them, 88% of them used polynucleotides in practice. The dermatologists said that their indications for using polynucleotides clinically were fine lines on the cheek followed by infraorbital fine lines, periorbital fine lines, uneven skin texture, dry skin, and fine lines on the forehead. They used a 33G needle and a serial puncture technique to inject the dermis. The most recommended protocol was a total of three sessions of polynucleotides which were spread across 4 weeks. 79% of the dermatologists used polynucleotides in combination with lasers and light therapy. The most popular being radiofrequency (non-invasive, needle RF) and high intensity focused ultrasound (HIFU). In conclusion, the authors have noted that use of polynucleotides is widely practiced among Korean dermatologists. According to their survey, the best indication for using polynucleotides is for facial fine lines, and as such, polynucleotides require numerous treatments and are often combined with a variety of non-surgical rejuvenation procedures. The authors hope that this data will help dermatologists to gain a better understanding of polynucleotides.
Efficacy of autologous platelet-rich plasma combined with negative pressure sealing drainage in the treatment of patients with diabetic foot ulcer
The aim of this study is to evaluate the efficacy of autologous platelet rich plasma (PRP) combined with negative pressure sealing drainage (NPSD) in the treatment of diabetic foot ulcers (DFU). To conduct this study, the authors carried out a comprehensive search using PubMed, Embase, Google Scholar, Cochrane Library and China National Knowledge Infrastructure. They also looked at Wanfang databases for randomised controlled trials (RCTs). This database included data up to November 2023, on the treatment of DFU using autologous PRP combined with NPSD. There was a total of two researchers who independently reviewed all of the literature and extracted data. They conducted quality assessments based on inclusion and exclusion criteria. The data analysis was performed using RevMan 5.4 software. There was also a total of 17 RCTs involving 1325 DFU patients that were included in the study. The results of the data showed that the use of autologous PRP combined with NPSD in DFU patients had significantly increased the ulcer healing rate. The results also showed that the treatment had significantly reduced the wound healing time. In conclusion, the authors state that this study had shown that the treatment of DFU with autologous PRP combined with NPSD accelerates wound healing, improves the overall treatment efficacy rate and offers a new option for the management of DFU.
Does injecting small amounts of fillers prevent the development of secondary blindness?
Dermal filler injections wrongly injected into the supratrochlear, supraorbital or dorsal nasal arteries could potentially result in an immediate loss of vision. The aim of this study was to identify how much filler injected could block the ophthalmic artery. For this study, 29 fresh cadavers were used. The authors looked at the arterial supply to the ophthalmic artery by dissecting the orbital area. They then injected 17 dermal filler injections into the supratrochlear, supraorbital and dorsal nasal arteries of each cadaver. The authors then looked at the amount of dermal filler injections that it took to block the ophthalmic artery. The authors noted that the supratrochlear, supraorbital and dorsal nasal arteries did not differ significantly. They concluded that a small amount of dermal filler injected can completely block the ophthalmic artery, resulting in visual loss.




