
In 2010, the US Food and Drug Administration (FDA) approved the use of botulinum toxins (BoTN) in the treatment of migraines and, one year later, the National Institute for Health and Care Excellence (NICE) approved it for the use in UK (NICE, 2012; Escher et al, 2016).
All the medical evidence proved that it is an effective way of treating this widely spread disease, which is rated as the seventh cause of medical disability worldwide.
Currently, the treatment is provided by some of the migraine clinics in the NHS, private GPs, neurologists and aesthetic practitioners.
History of migraine
The word ‘migraine’ derives from the Greek word ‘hemicrania’ (imikrania; ημικρ ανία), which means ‘half the skull’, as, typically, most patients have unilateral headaches. With the new diagnosis criteria, migraine could be all over the head, lasting for few hours or days (Rose, 1995).
In 400 BC, Hippocrates described in detail the occurrence of migraine attacks, including the visual disturbances during migraine, the aura and the relief from vomiting. The word ‘migraina’ (ημικρανία) was later established by the Greek physician Κλαύδιος Γαληνός (Galen of Pergamon) (Rose, 1995).
In prehistoric times, migraine was treated with trepanning, a surgical procedure that involves drilling a hole in the skull to release the evil spirits from the head (Rose, 1995).
Prevalence of migraine
Migraine is the third most prevalent disease worldwide and, unfortunately, it is under-diagnosed but awareness is increasing (Natoli et al, 2015). Even many medically qualified people do not know about the use of BoTN in migraine treatment, as the author was informed by many GPs.
Migraines affects around 2% of the world population (Natoli et al, 2010) and are more prevalent than diabetis, epilepsy and asthma combined (Primary Headache Disorders, 2010).
In the UK, NICE has estimated that there are 6 million people who suffer from migraines, with 190 000 migraine attacks per day with more prevalence in women than men (Steiner et al, 2003).
New methods and criteria to diagnose migraines have been developed, so it is expected that the next statistics will show a higher number of people suffering from this condition.
Effect of migraine on life quality and disability
It is estimated that the UK population loses 25 million days from work or school each year due to migraines (Steiner et al, 2003).
Migraines/chronic headaches were found to be the second most frequently identified cause of short-term absence (47%) for non-manual employees. (CBI and Pfizer, 2011).
Migraine has an enormous disabling effect of every aspect of life for those who suffer from them, affecting their physical, social, emotional and working life. It can lead to:
- Missing household activity such as shopping and housework
- Parental difficulty, i.e. looking after children
- Depression and low mood
- Missing social, family and leisure activity
- Absence from work.
BoTN in medicine
The word ‘botulinum’ comes from the Latin word ‘botulus’, which means sausage. In the 18th century, it was noted that food poisoning ‘botulism’ was related to eating rotten sausages. Those patients who developed botulus were noticed to have muscle weakness (Aronson, 1997; Torrens, 1998).
In 1946, Mr Burgeon, a British investigator, discovered that BoTN produced clostridium botulinum (causes botulus), a rod-shaped gram-positive bacterium, causing muscle weakness that was laer used to treat certain medical conditions, beginning with chorea (abnormal involuntary disorder) (Drachman, 1964).
These muscle weakness properties were further studied, and experiments on certain medical conditions were carried out until 1980, when the FDA gave its first approval to treat strabismus, blepharospasm and hemifacial spasm (Scott, 1980).
In 1989, Dr Alan Scott, an American ophthalmologist and pioneer in using BoTN in medical treatments, treated a patient with unilateral blepharospasm (Jabbari, 2016). The patient visited him 2 weeks later asking him to inject her other eye, as the crow's feet in the treated eye had improved. So, he treated her and that was the first aesthetic use of BoTN, which later on boomed and became one of the most profitable expanding business of the new century. He also noticed there was improvement in patients' headaches after having BoTN treatments.
Further studies were conducted on BoTN and its medical uses until 1990, where studies provided evidence that BoTN can block neurotransmitters involved in pain pathways, which Dr Silberstein used in 2000 to provide the first trial for BoTN injections in migraine patients (Silberstein et al, 2000). It later became one of the most effective treatments for migraine, which led to the FDA and NICE approving it (Silberstein et al, 2000).
BoTN in treating migraine
The International Classification of Headaches disorder in the third conference (ICHD-3) classified migraine into acute and chronic and no longer used the terms migraine with or without aura. Chronic migraines are defined as having 15 headaches per month (NICE, 2012).
Only chronic migraine is treated in the NHS for those patients who fail to respond to three preventive medications and there is a waiting list that can exceed 18 months. In the UK, migraines are estimated to cost the NHS £150 million per year, mostly from the costs of prescription drugs and GP visits (All-Party Parliamentary Group on Primary Headache Disorders, 2010). There are around 17 NHS nurses in the UK who provide the injections in migraine clinics, which adds to the waiting time.
Although it is evidence-based medicine, not enough medical professionals are trained to provide it in the NHS, which only provides it for chronic migraines, rather than episodic.
Most migraine patients (chronic and episodic) who are treated by aesthetic practitioners provide it privately. The author could not find any formal statistics about BoTN for migraine in the private or aesthetic sector.
Pathophysiology of migraine
Migraine results from excessive external stimulus as stress, light, sound cold that sends extensive pain signals by the trigeminal nerve to the pain center in the brain leading to a migraine attack.
BoTN tends to block these signals by preventing the sensory nerve from being stimulated from the start.
How BoTN works on migraines
The way BoTN works to treat migraine is fairly similar to its effect on muscle relaxation, with some differences.
BoTN in the muscle
In normal muscle contraction (Figure 1), the vesicle in the presynaptic nerve terminal secrets acetylcholine (AcH) in response to a stimulus to attach to the receptor in the post-synaptic muscle terminal, leading to muscle contraction. For the vesicle to secrete the AcH, it contains it needs the help of snare 25 (yellow-coloured arm) of the snare complex to facilitate the fusion.
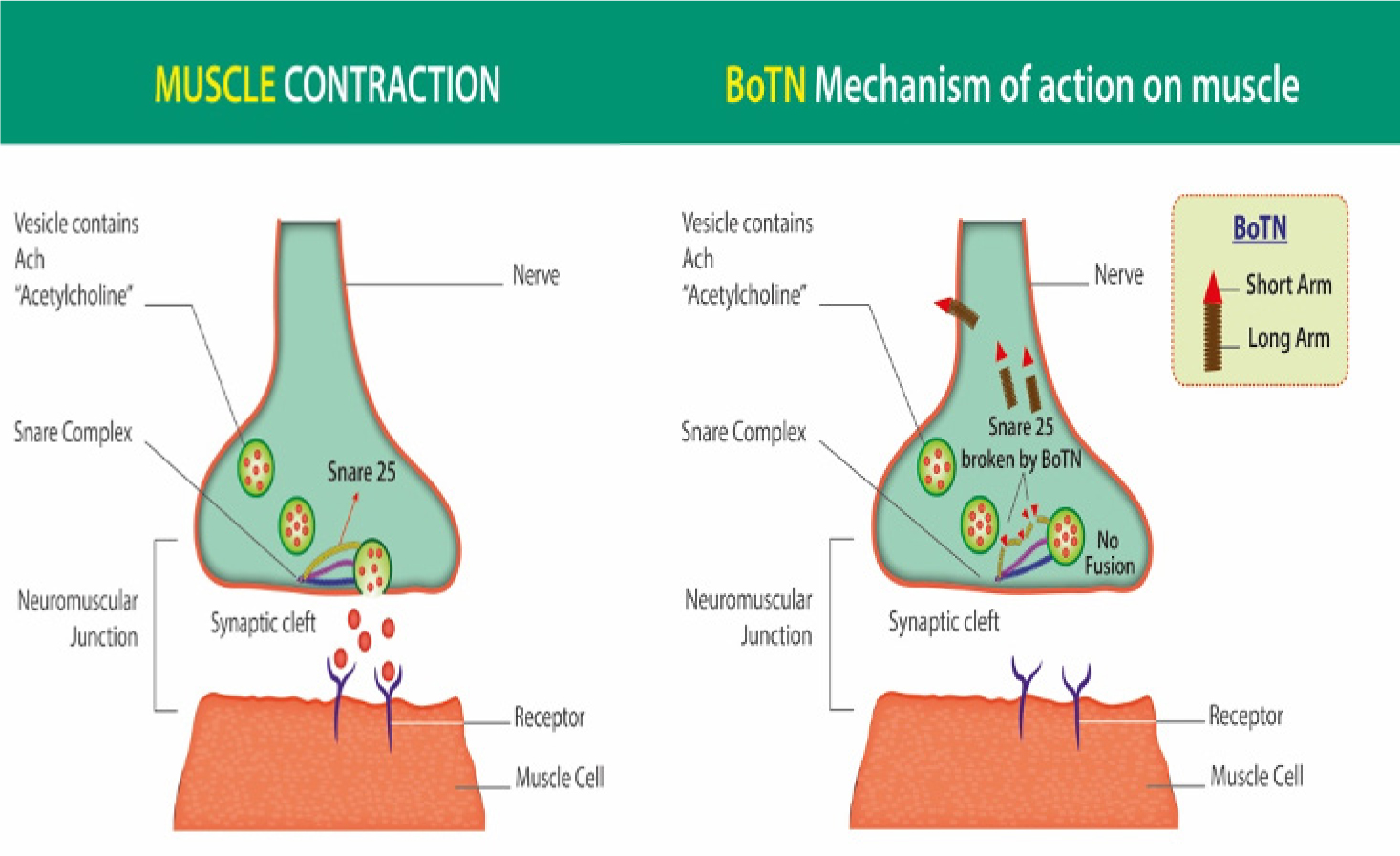 Figures 1 and 2. Muscle contraction and BoTN's mechanism of action on muscle
Figures 1 and 2. Muscle contraction and BoTN's mechanism of action on muscle
BoTN destroys the snare 25 (Figure 2), so the vesicles cannot secrete it AcH to its receptors in the muscle, which prevent muscle contraction. This is the basis of how BoTN is used in aesthetics for wrinkle treatment.
BoTN on nerve cells
There are some differences between the muscle and the nerves involved in generating the attach.
If looking at Figure 3 and comparing it to Figure 1, some differences can be noted:
- In the post-synaptic junction, there is a nerve, rather than a muscle
- The neurotransmitter in the vesicles are glutamate and Calcitonin gene-related peptide (CGRP), compared to AcH in muscle endplate.
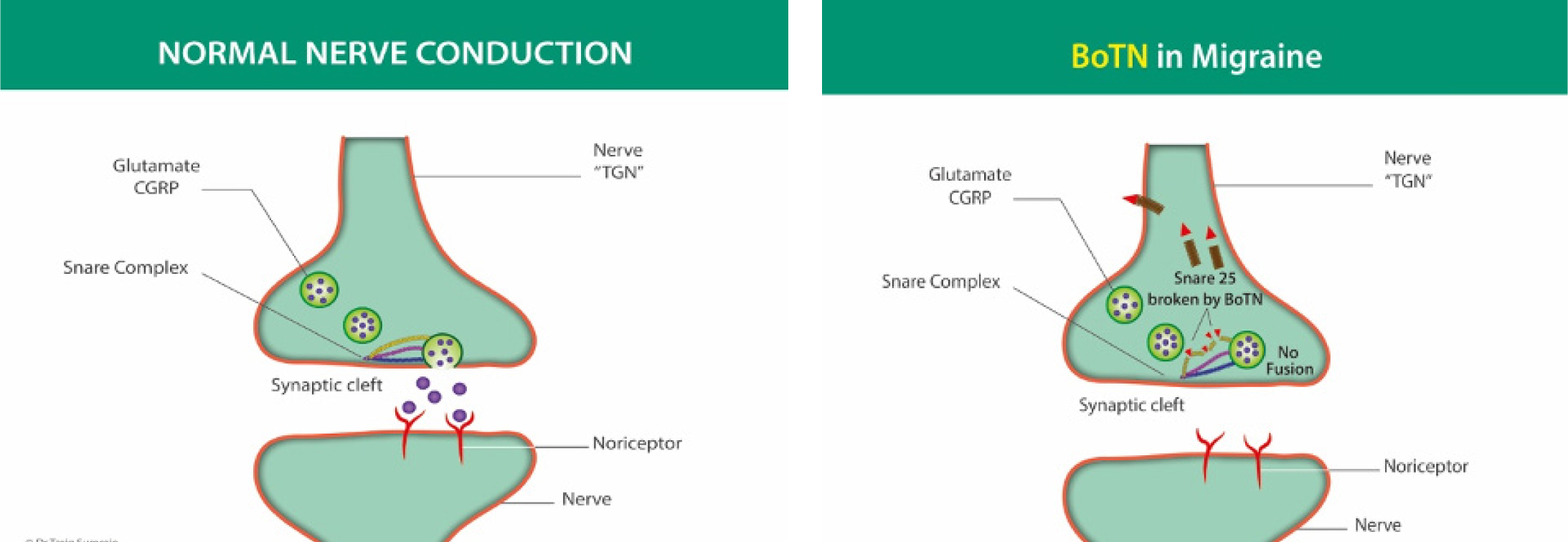 Figures 3 and 4. Normal nerve conduction and BoTN in migraine
Figures 3 and 4. Normal nerve conduction and BoTN in migraine
The action of BoTN on the nerve after injection is the same (Figure 4). The AcH destroys snare 25 so that it can no longer secrete its neurotransmitter CGRP and Glutamate to the post-synaptic receptor, so the migraine pain impulses to the brain is stopped and we no longer have a migraine attack.
What the evidence says
A common question received when presenting BoTN for treating migraine is what evidence there is. Figure 5 explains the post-treatment results and how BoTN is effective in treating migraines.
 Figure 5. Results of treating migraine with BoTN
Figure 5. Results of treating migraine with BoTN
Injecting techniques
There is a major difference between injecting the face for anti-wrinkles and treating migraines. This is important to understand, as many of the experienced practitioners who attend the author's migraine course stated: ‘I inject the procerus, frontalis and masseter muscle for migraine’.
Since the masseter has no role in the pathophysiology of migraine, there is no need for it to be injected. As this is a common practice, it is important to detail on where should be injected.
In anti-wrinkle treatments, specific muscles are being targeted, while in treating migraine, specific nerves are targeted. There are specific landmarks and injection techniques that need to be established.
Figure 6 show some of the differences in injection landmarks between aesthetic injections and migraine injections.
 Figure 6. Anatomy and injection landmarks
Figure 6. Anatomy and injection landmarks
From Figure 6, it can be noted that, when injecting the procerus muscle for migraine, it is at the same level of the medial heads of the corrugator and superficial as the infratrochlear nerve (branch of the nasociliary nerve which originates from the trigeminal nerve) is most superficial here, compared to the deeper, inferior injection when treating the frown.
Another difference noted when injecting the forehead is that the injection is given high up and just below the hair line and medially, as the terminals of the supraorbital and supratrochlear nerves are located, which are the target, and not the frontalis muscle itself.
In treating migraine, the whole of the scalp is treated in specific landmarks and injection techniques target all those nerves involved in the pathophysiology of migraine (the face, temporals, occipitals and neck).
Figure 7 shows the nerves targeted in the occipital area of the head.
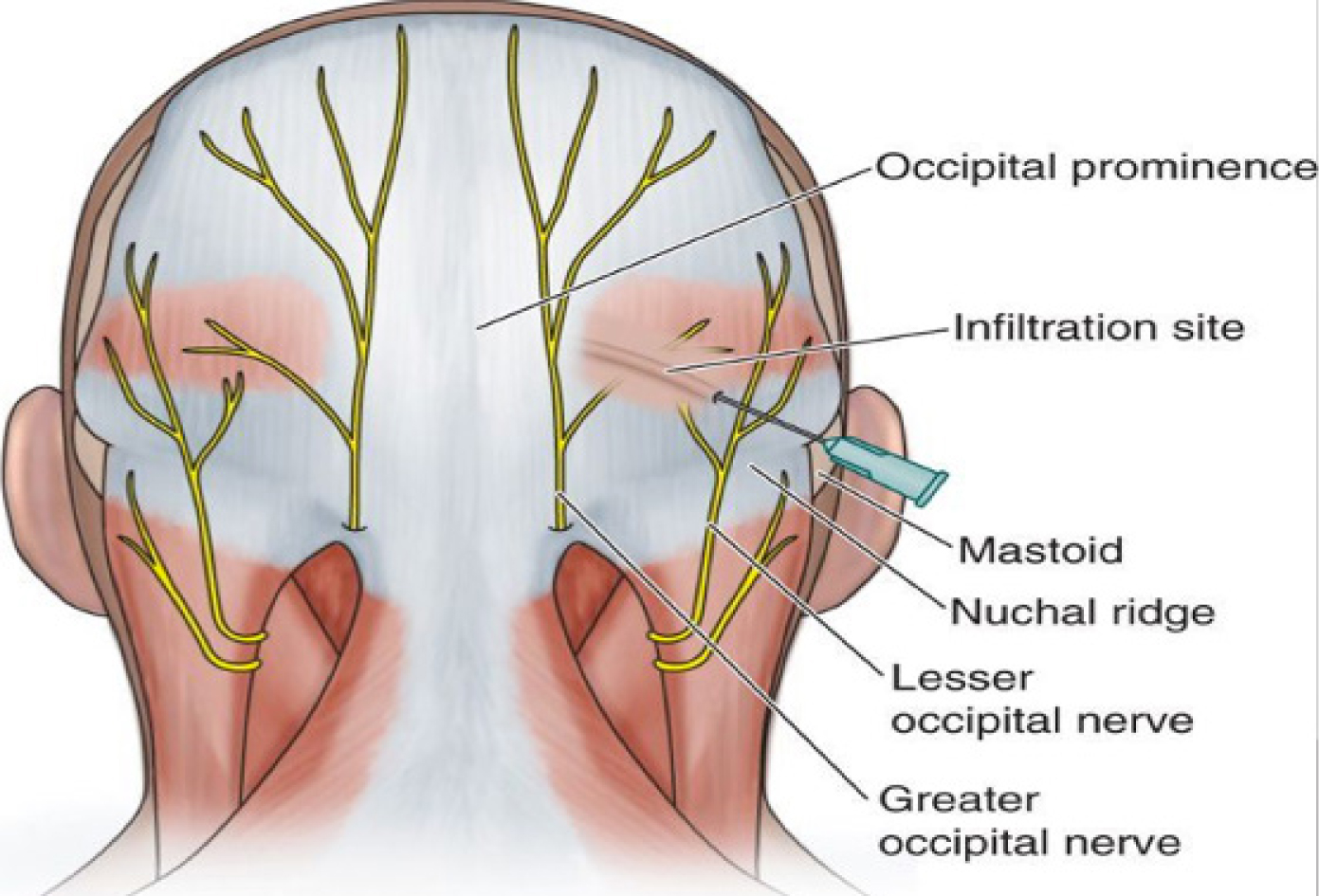 Figure 7. Nerves in the occipital area
Figure 7. Nerves in the occipital area
Aesthetic practitioners and migraine
So, how are migraines confirmed or diagnosed before the aesthetic practitioner carries out the treatment? Simply, aesthetic practitioners do not diagnose migraines. The diagnosis is made by the patient's GP or neurologist and only those known to suffer from and already diagnosed with migraine are treated.
There are around six million migraine patients in UK, with 190 000 daily migraine attacks (NICE, 2011). Those patients are already diagnosed with migraine, and most of them have suffered from migraines for years. It is extremely unlikely that a patient with a new onset headache will come to an aesthetic practitioner for that problem—they would visit their GP first.
Future uses of BoTN in medicine
There are over 1000 medical uses of BoTN in medicine. Some conditions that are approved by the NHS for BoTN use are:
- Migraines
- Hyperhidrosis
- Bruxism
- Irritable bladder
- Spasticity
Furthermore, some of the new areas for treatment that are being developed are:
- Back pain: recent research has shown that, if the correct doses in the correct landmarks were injected, very good results can be received (Waseem et al, 2011). Some trust is already providing this treatment
- Depression: recent studies supported by MRI studies show that patients already diagnosed with depression and who take anti-depressants show improvement on their anti-depressant scores after having the BoTN in the frown area (procerus and head of corrugator) (Wollmer et al, 2012)
- Atrial fibrillation: mainly preventing AF post cardiac surgery and is injected during surgery
- Pain relief: especially in cancer patients as they develop neuropathic pain.
Summary
BoTN for migraine is evidence-based medicine approved by NICE and the FDA. It gives great relief to patients and dramatically improves their quality of life and changes it to the better.



