

Combining topical dermal infused exosomes with injected calcium hydroxylapatite for enhanced tissue biostimulation
Research into exosomes—tiny, sac-resembling structures formed inside cells—is growing rapidly. Exosomes transfer information between cells by delivering signalling molecules. With regard to its use, there are studies looking at combination treatments using exosomes for the purpose of biostimulation. It can also be used in treatments involving calcium hydroxylapatite (CaHA), platelet-rich plasma and platelet-rich fibrin matrix.
The aim of this study was to create safe protocols for improving the delivery of topical exosomes to enhance the quality of the skin, either by using them in a standalone treatment or in combination with injectable CaHA.
A total of 40 patients were involved. To test if the method alone would allow exosomes absorption, 20 of them had facial biostimulatory dermal infusion; five of them had facial bio stimulator infusion followed by CaHA injection to their faces; five others had exosome biostimulatory dermal infusion followed by hyperdiluted CaHA injection to their necks; five more had facial dilute CaHA injection without dermal infusion; the remaining five had their necks injected with hyperdiluted CaHA injection without dermal infusion.
All patients included in the study had a Quantificare 3-D photo-documentation and skin analysis conducted prior to treatment. All had their skin cleansed with a gentle glycolic acid facial wash. To induce a ‘homing inflammatory environment’ for the exosomes, a sea salt exfoliation was performed and a nitric oxide serum was then applied to the skin. A 3 MHz ultrasound was then used to increase the absorption of the nitric oxide serum.
A topical paste that contained equal amounts of exosomes—25 units of botulinum toxin and hyaluronic acid—was mixed altogether in a 3ml syringe. This paste was then applied evenly to the treatment areas. The cavitating ultrasound was used to further help with the absorption of the paste. All of the patients were then treated with LED therapy.
Reviews of each patient took place at days 15 and 30 after the treatment. The results showed that all the dermal infusions used as standalone and CaHA injection used as standalone showed an improvement in the tone, quality, as well as the texture of participants' skin.
Quantificare results showed improvements to wrinkles, pores, skin tone, improved vascularity and a reduction in oiliness and pigmentation. Furthermore, results were enhanced when the skin primer was applied prior to injections of CaHA.
In conclusion, using topical placental mesenchymal stem cell-derived exosomes into treatment menus can give enhanced results on the skin. Exosomes can be used as a standalone treatment or combined with other treatment modalities such as botulinum toxin, hyaluronic acid dermal filler, and CaHA to create a bespoke treatment based on each individual's needs with their skin.
It was also noted that the topical absorption of exosomes was enhanced with sea salt exfoliation, a topical nitric oxide-generating serum, and a 3 MHz cavitating ultrasound. Finally, the addition of CaHA injections following topical exosomes significantly enhanced the quality of the skin—at a rate faster than using either as a standalone treatment.
Effect of vitamin D supplementation on psoriasis severity in patients with lower-range serum 25-hydroxyvitamin D levels
A routine treatment for those suffering with psoriasis—an autoimmune condition causing flaky patches of skin—is using topical vitamin D. To date, there has been no research examining the effects that taking oral supplements may have on psoriasis.
In light of this niche, the aim of this study was to explore the effect that vitamin D supplements have on psoriasis during the winter months. To conduct this study, the authors carried out a randomised, double-blinded placebo-controlled trial, involving two parallel groups.
This study was conducted for two winter seasons—from 2017 to 2018 in the first instance and from 2018 to 2019 in the second. A total of 122 participants joined the study—46 of whom were women and 76 men. 60 of the participants were randomly selected to join the vitamin D group and the other 62 were placed in the placebo group.
The study was carried out by the clinical research team at the University Hospital of North Norway. All adults that had active plaque psoriasis, and 25-hydroxyvitamin D levels of less than 24 ng/mL were included in the study. The two groups either had vitamin D or a placebo for a period of 4 months in total.
The authors noted that after this study there was no difference noted in the change in Psoriasis Area and Severity Index (PASI) score between both groups. In addition, it was noted that there was also no difference in the change in Physician Global Assessment score, self-administered PASI or Dermatology Life Quality Index between both of the groups.
In conclusion, the results evinced that taking vitamin D supplements posed no further effect on the severity of psoriasis.
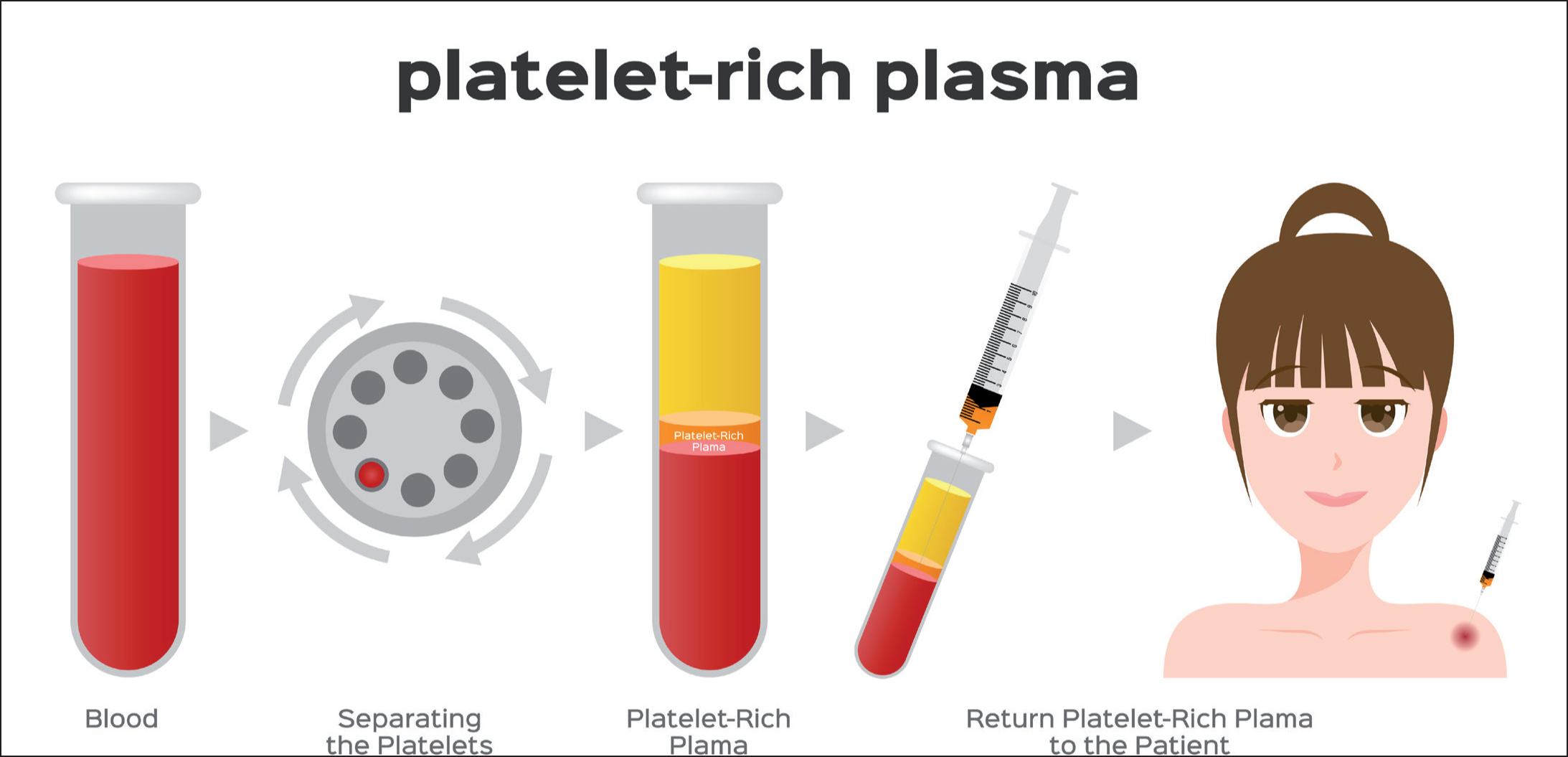
A new technique for separating platelet-rich plasma by a copolymer device without a centrifugation process
Platelet-rich plasma (PRP) is involved in a variety of medical applications globally. In aesthetics, it can be applied in therapy for acne scars, hair loss, cicatrix and wrinkles. The current PRP kits available, however, all require the use of a centrifuge to separate the plasma from the red blood cells.
In this study, the authors trialled a new method to separate the platelets. By using a cationic copolymer (i.e., water-soluble polymer) coating on a polyurethane sponge, the authors were able to obtain platelet separation from the red blood cells.
They were able to evaluate the efficiency of this new method of PRP preparation. In comparison with that of a well-known available kit (RegenKit-THT) and centrifugation, the quantification of red blood cells, white blood cells, and platelets were higher with this novel method.
The authors research found that the copolymer showed no hemolysis (i.e., destruction of red blood cells) and no cytotoxicity against cell viability.
The authors also showed that the PRP collected using this copolymer device contained a high concentration of PRP platelets and angiogenic growth factors (i.e., formation of red blood cells). Further research showed that the separated PRP also had beneficial effects on cell migration, angiogenesis, and matrix metalloproteinase gene expression. Following these results, the authors have now developed a cationic copolymer-coated PU sponge as a PRP preparation device without the need for any centrifugation during preparation.
» They were able to evaluate the efficiency of this new method of PRP preparation. In comparison with that of a well-known available kit (RegenKit-THT) and centrifugation, the quantification of red blood cells, white blood cells, and platelets were higher with this novel method «
Nutraceutical strategies for alleviation of UVB phototoxicity
Exposure of UVB rays to the keratinocytes (i.e., the most dominant cell type that makes up the epidermis) can cause carcinogenesis. This can occur when the pyrimidine dimer lesions in DNA—which suppresses biological repair mechanisms required to fix the lesions—inhibits the apoptosis (i.e., programmed cell death) required for the elimination of initiated cells. This, then, causes cancerous cell proliferation.
The authors explored some nutraceuticals, most commonly spirulina (i.e., a greenish dietary supplement), soy isoflavones, long-chain omega-3 fatty acids, the green tea catechin epigallocatechin gallate and Polypodium leucotomos extract. Each of these have all been shown to resist photocarcinogenesis (i.e., a sequence of biochemical events that lead to skin cancer). As seen in an experiment of UVB-exposed hairless mice, the authors have concluded that these nutraceuticals can have an impact on sunburn and photoaging.
While further research is needed, the authors believe that given the positive benefits for the use of nutraceuticals on photocarcinogenesis, sunburn, and photoaging, the results appear promising for the future.



