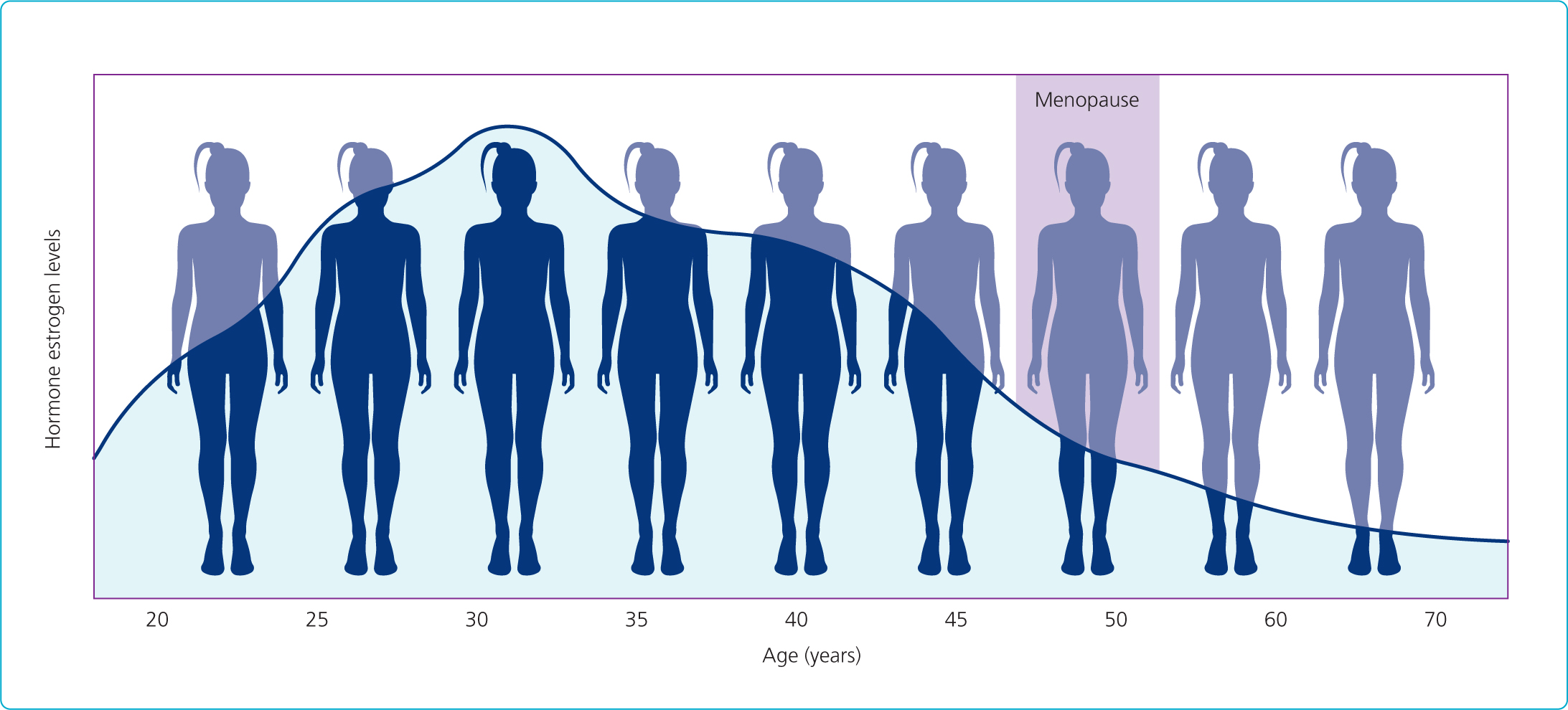
Oestrogen plays a critical role in maintaining skin thickness and elasticity by promoting the production of collagen and elastin. As oestrogen levels decline during menopause, the epidermis and dermis become thinner, resulting in reduced collagen and elastin levels. This leads to a loss of skin elasticity and firmness. Or as Wilkinson et al (2021) stated, oestrogen deficiency results in significant thinning of the epidermis and dermis, and a reduction in collagen and elastin, which contributes to the appearance of wrinkles and sagging skin. Additionally, the decrease in oestrogen affects the skin's hydration levels, exacerbating dryness and making the skin more prone to damage from environmental factors like UV radiation, leading to conditions such as solar elastosis.
Hot flushes and sweats
These are common symptoms of menopause caused by hormonal fluctuations affecting the functioning of the hypothalamus. Hot flushes are experienced by up to 75% of perimenopausal women and are linked to oestrogen withdrawal (Freeman, 2018).
Itching and dryness
Reduced oestrogen levels impair the skin's ability to retain moisture, alongside flushes and sweats contributing to insensible water loss, leading to dryness, itching and irritation. Oestrogen helps maintain skin moisture by increasing the production of hyaluronic acid, a key molecule involved in skin hydration (Verdier-Sévrain and Bonté, 2007).
Anxiety and gut health
Hormonal changes can also impact mental health, with anxiety being an extremely common symptom. The gut microbiome, which plays a crucial role in nutrient absorption and overall health, is often disrupted during menopause, further affecting skin and mental health. There is a growing body of evidence linking gut health to skin health, and disruptions in the gut microbiome can exacerbate skin conditions (Bowe and Logan, 2011).
Menopausal women often experience an array of skin disorders. These can include:
Increased melanogenesis
Leads to pigmentation issues.
Solar elastosis
Caused by long-term sun exposure, resulting in damaged elastic fibres.
Rosacea and other functional disorders
Rosacea is a chronic inflammatory condition that can be aggravated by hormonal fluctuations and gut health disturbances (Gether et al, 2018). It can be a very distressing condition for the sufferer who, not only feels very sore but often suffers a decrease in confidence and self-esteem due to the very visible nature of the key symptom.
Reduced sebum production
Leads to decreased hydration and weakened skin barrier function.
Increased histamine response
During menopause, changes in histamine levels can significantly impact the skin, contributing to increased sensitivity and various dermatological issues. Histamine is a biogenic amine involved in immune responses, and its regulation is influenced by oestrogen levels. As oestrogen declines during menopause, there is a dysregulation of histamine, often leading to an increased histamine response. This heightened response can manifest as greater skin reactivity and susceptibility to irritants, resulting in symptoms such as itching, redness, and swelling. Additionally, higher histamine levels can exacerbate conditions like rosacea and eczema, causing more frequent and severe flare-ups. The increased histamine can also impair the skin barrier function, reducing its ability to retain moisture and protect against environmental stressors, thereby promoting dryness and irritation. Consequently, managing histamine levels and addressing histamine sensitivity becomes crucial in the skincare regimen for menopausal women to alleviate discomfort and maintain skin health (O'Mahoney, 2011).


Multimodal interventions
Approaching treatment planning in a systematic manner helps with developing a comprehensive care plan. Looking at topicals, systemic treatments, medical aesthetics and lifestyle modifications helps us to provide a more holistic overview and can assist with patient compliance.
Typically, topical treatments might include:
Niacinamide (vitamin B3)
Niacinamide helps in reducing inflammation and improving the skin barrier. Nicotinamide increases the biosynthesis of ceramides as well as other stratum corneum lipids, thereby improving the epidermal permeability barrier (Surjana et al, 2012).
Vitamin A (retinoids)
Vitamin A/retinoids promote cell turnover and collagen production. Retinoids are effective in promoting collagen synthesis and improving the appearance of fine lines and wrinkles (Kafi et al, 2007).
Vitamin C and antioxidants
Vitamin C and antioxidants protect against oxidative stress and promote collagen synthesis. Topical vitamin C is a potent antioxidant that can neutralise free radicals and stimulate collagen production (Pullar et al, 2017).
Tyrosinase inhibitors
Tyrosinase inhibitors help reduce hyperpigmentation.
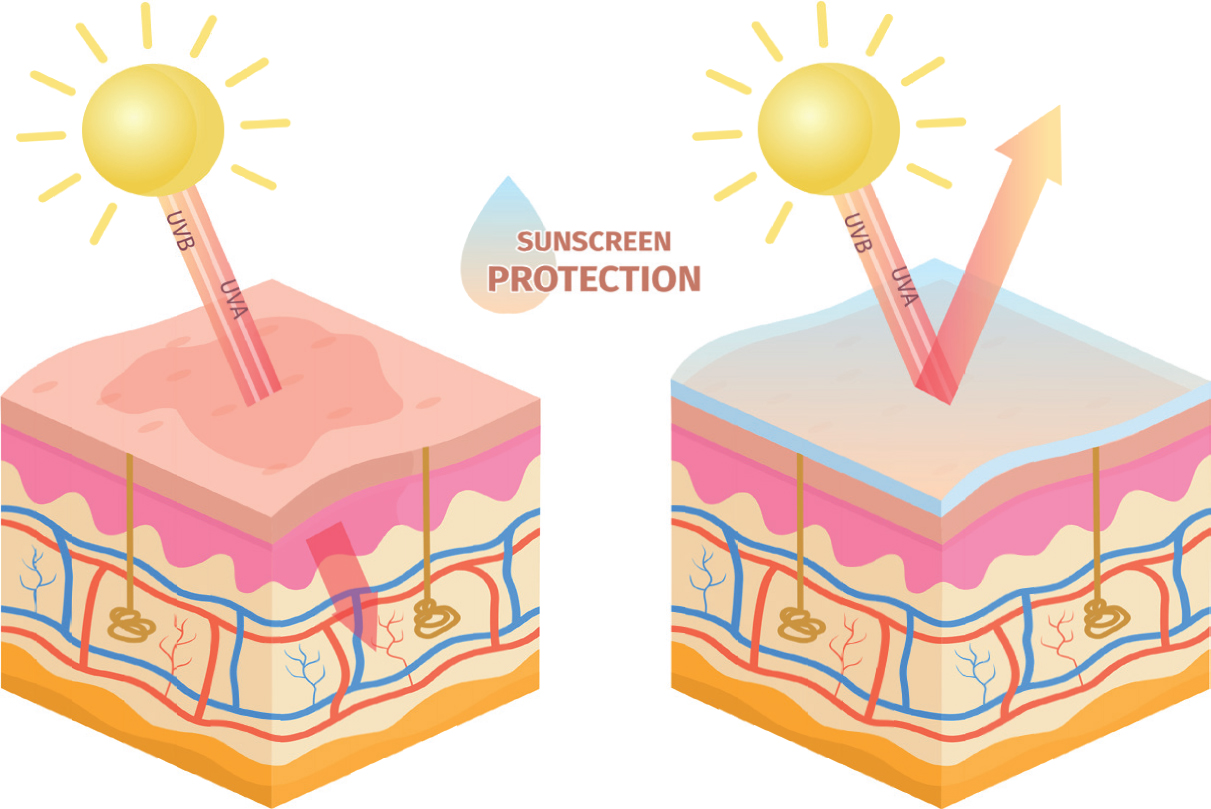
Sun protection factor (SPF)
SPF is essential for protecting against UV damage.
Systemic treatments which were advised are:
Hormone replacement therapy (HRT)
Can mitigate some menopausal symptoms and improve skin thickness and hydration. HRT can help restore skin hydration and thickness, thereby reducing the appearance of fine lines and wrinkles (Sator et al, 2001).
Pre and probiotics
Pre and probiotics support gut health, which is closely linked to skin health. A healthy gut microbiome enhances nutrient absorption and reduces inflammation. Probiotics have been shown to positively affect the gut microbiome, which in turn can improve skin health by reducing inflammation (Bowe and Logan, 2011).
Lifestyle modifications
Stress management, regular sleep and an anti-inflammatory diet can significantly improve skin health. Stress reduction techniques such as mindfulness and yoga can significantly lower cortisol levels, thus benefiting both mental and skin health (Goyal et al, 2014).
Reducing stimulants
Limiting caffeine, alcohol and sugar intake can reduce skin inflammation and breakouts.
Considering gut health alongside mental health is also of vital importance. The Gut-Brain-Skin Axis theory states that gut health significantly influences both mental health and skin conditions. Disruptions in the gut microbiome can lead to systemic inflammation, which not only affects skin health but also contributes to mental health disorders such as anxiety and depression. Gut microbiota play a crucial role in the regulation of immune responses and systemic inflammation, which are linked to skin health and mental wellbeing (Bowe and Logan, 2011). Studies have shown that probiotics can improve both gut health and symptoms of anxiety and depression, which in turn can enhance skin health by reducing stress-induced skin issues. Restoring gut microbiota balance through probiotics can significantly reduce skin inflammation and improve skin barrier function (Sivamaruthi et al, 2015).
Research has demonstrated that menopausal women often experience a decline in gut microbiota diversity, which correlates with increased systemic inflammation and exacerbation of skin conditions such as rosacea and eczema. Probiotic supplementation has been shown to restore gut microbiota balance, improve skin barrier function and reduce inflammation, thereby improving both mental and skin health (Bowe and Logan, 2011).

Practical application of these theories and approach are evidenced in the case study below.
Case study
Patient background
A 52-year-old woman working in a high-stress healthcare environment presented with severe rosacea. She reported irregular meal times, a lack of a consistent daily routine, and high levels of work-related stress. Her main skin concerns included persistent facial redness, frequent flare-ups, and increased sensitivity to her skincare and cosmetics.
The patient underwent a comprehensive assessment that included a detailed skin examination, medical history review and lifestyle evaluation.

Key findings include:
The treatment plan was designed to address the multifaceted nature of her symptoms, focusing on skin health, gut health and overall wellbeing. This is approached in a systematic manner.
Topical treatments – use products containing:
Recommended systemic treatments
Lifestyle modifications
Stress management
Suggested incorporating stress reduction techniques, such as deep breathing exercises and meditation to reduce stress and anxiety. Mindfulness-based stress reduction has been shown to significantly lower cortisol levels and improve both mental and skin health (Goyal et al, 2014).

Regular sleep schedule
Emphasised the importance of maintaining a consistent sleep schedule and aiming for 7-8 hours of quality sleep per night. Adequate sleep is essential for skin health and overall wellbeing (Sweity et al, 2015).
Hydration
Encouraged adequate water intake to maintain skin hydration and overall health. Proper hydration is crucial for maintaining skin elasticity and reducing the appearance of fine lines (Palma et al, 2015).
Regular physical activity
Recommended incorporating regular, moderate exercise (such as yoga and walking) to improve overall wellbeing and reduce stress. Regular physical activity can enhance skin health by improving circulation and reducing inflammation (You and Nicklas, 2008).
Results
Over a 12-week period, the patient reported significant improvements in her skin condition and overall wellbeing.
She experienced:
Conclusion
This case study highlights the importance of a holistic, multimodal approach to managing skin conditions during menopause. By addressing skin health, gut health, and overall wellbeing, it is possible to achieve significantly greater improvements in skin condition and quality of life for menopausal women than could be achieved with medical aesthetic and skin treatments alone. As this case demonstrates, a combination of topical treatments, systemic interventions and lifestyle modifications can provide effective relief from menopausal skin symptoms and enhance overall health, wellbeing, confidence and self-esteem for patients undergoing an often, particularly challenging, phase of life.