 Dr Irfan Mian
Dr Irfan Mian
Non-surgical repositioning of the face, neck and other parts of the body's tissues can be achieved using a variety of materials. Repositioning of the tissues using threads is a more accurate term than ‘tissue-lifting’, which is in common use. However, the latter term will be used in this article, and the reader should be aware of the subtle difference.
The threads that are referred to in this article are made of polydioxanone (PDO)—a safe and bio-compatible material that has a long history of use in surgery (Suh et al, 2015). PDO threads have been shown to give great clinical results, with a high degree of satisfaction from both the patient and the clinician (Unal et al, 2019).
To understand how tissue-lifting threads work and allow the facial tissues to ‘slide’ in the desired direction, an understanding of the facial vector forces and cellular remodeling factors is needed. These factors will determine the direction, number, type and size of thread to be used, so that the best tissue lift is achieved.
Vector forces
Thread vectors can be macro-forces, designed to oppose the gravitational downward migration of the tissues of the face, neck and body, or smaller micro-forces, which may or may not be significant.
In regard to molded PDO threads, there are two vector forces. The first is the major vector force, which is in the longitudinal plane running the length of the thread, and the second is the minor vector, running 90 degrees to the former, concentrically.
What are vectors?
Vector quantity forces have both direction and magnitude. A vector quantity without direction and only magnitude is known as a scaler. In thread placement situations, the resultant vector is affected by multiple factors that may be in play at the site. They can be classed as primary vectors, which relate to the thread itself, or secondary vectors, which relate to other structures. These vector forces are further modified by extrinsic and extrinsic ageing of the facial tissues of both the soft and hard tissue and remodeling of areolar connective tissue at a cellular level.
There are also differences in male and female patients. Additionally, the presence of any pathological conditions that may need therapy or may, indeed, be a contraindication for any thread procedure.
After the initial mechanical displacement or ‘lift’, thread placement results in the activation of parts of the immune system. This is similar to the effects of placing a needle in acupuncture, creating a wound that starts a cascade of ‘wound healing’ reactions.
Immune system overview
As a result of cytokine production, there are many stimulatory effects from cells of the immune system. This chemical transmission of information and the resultant reparative response is called mechanotransduction. For example, the interleukin group of proteins mediate communication between cells as a result of cytokine release. Interleukin 1, produced by macrophages, induces Interleukin 2 production from the T cell leukocytes. This forms the basis of the immunogenic response.
Mechanotransduction
Mechanotransduction is the conversion of mechanical stimuli into electrochemical activity and takes place in many body processes. In the context of thread-lifting, the concern is with mechanotransduction commencing the wound healing cascade. Immediately after disruption or wounding, in this case with PDO threads, the process of wound-healing begins, bringing together numerous cell types to collaborate in several sequential phases (Kuehlmann et al, 2020).
Langevin et al (2006) demonstrated that the effect of the acupuncture needle rotation was quantifiable by morphometric analysis of mouse tissue explants imaged with confocal microscopy. Fibroblasts spread extensively and changed their morphology, resulting in lamellipodia formation via cellular mechanotransduction (Langevin et al, 2006).
Thread placement with, for example, PDO threads acts similarly to acupuncture and will result in an inflammatory response that is in line with the general health of the individual and their biological age. With the onset of ageing and other factors, a reduced response of the immune system is usually found.
Mechanotransduction is important because it is one of the major factors that contributes to the behaviour of the morphological fibroblast at a cellular level, which determines neocollagenesis.
By changing shape, fibroblasts can dynamically modulate the visco-elastic behaviour of areolar connective tissue. This is through rho-dependent cytoskeletal mechanisms, which influence the dynamic interplay of forces contributing to the thread-induced vectors at a cellular level (Langevin et al, 2006).
As the degree of mechanotransduction varies, it is difficult to predict the final aesthetic outcome of thread placement at the time of the treatment. Mechanotransduction factors and healing take several weeks to peak. This, coupled with immediate and late wound healing at a cellular level, will provide the factors that determine the final repositioning of the tissues. In clinical practice, this is in approximately 3 months in otherwise healthy individuals in most cases.
Vector forces as a result of thread placement are also influenced by the anatomy of the area to be treated. For example, in the face, true and false ligaments play a key role in the resultant vector force production.
Anatomy of facial ligaments
True ligaments are ligaments that connect the dermis to the underlying periosteum, while false ligaments are diffuse condensations of fibrous tissue that connect superficial and deep facial fascia. True ligaments are the zygomatic-orbital- and mandibular-retaining ligaments and are shown in Figure 1 as Z, O and M, respectively. False ligaments are nasolabial, masseteric and pre-auricular ligaments and are detailed in Figure 1 as N, M and P.
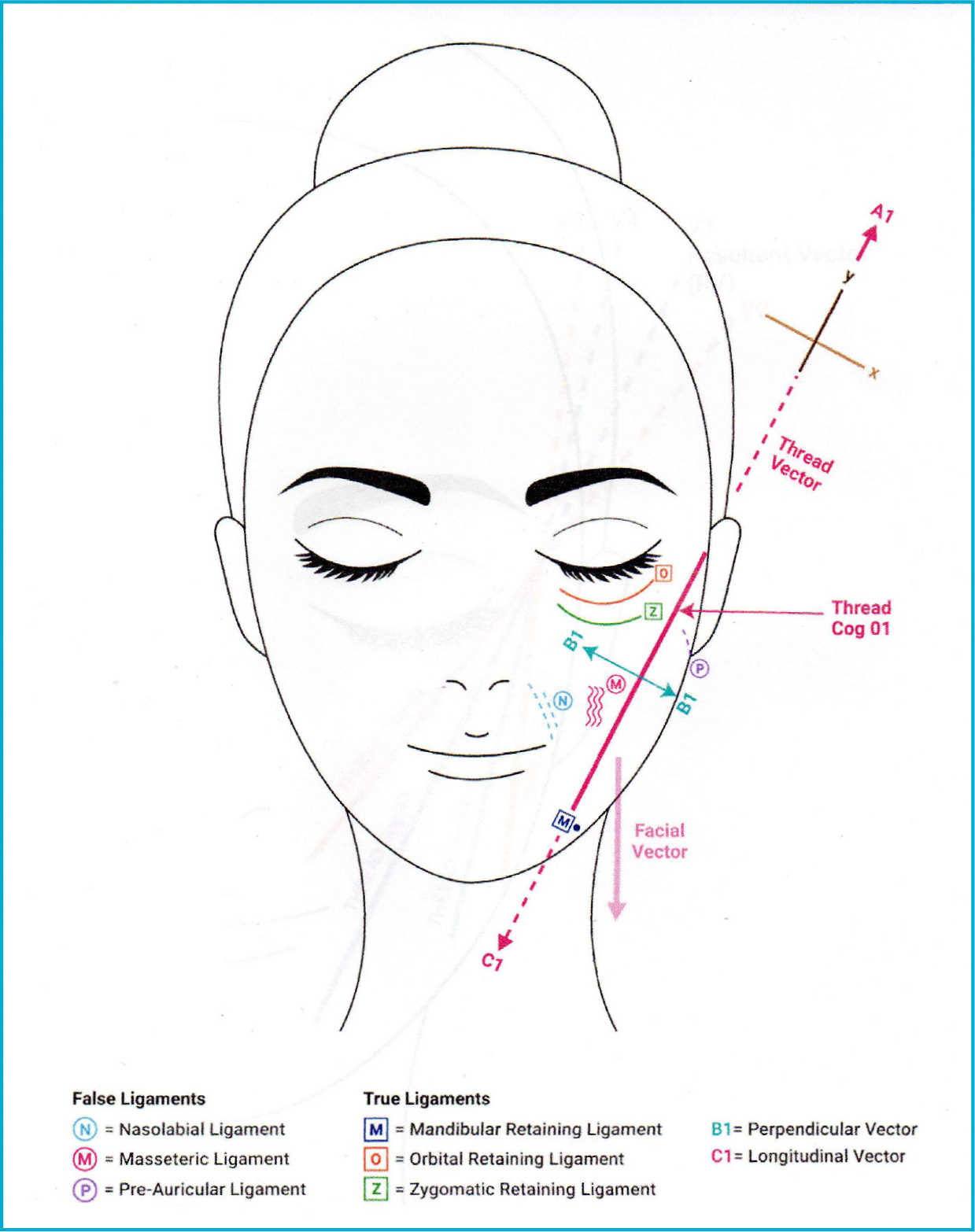 Figure 1. True and false ligaments
Figure 1. True and false ligaments
The true ligament and the zygomatic-retaining ligament connects the inferior zygomatic arch border to the dermis. Its anatomical site is a little posterior to the origin of zygomaticus minor muscle.
In clinical practice involving lifting threads, true ligaments have a major influence on the direction and magnitude of the vector forces. They oppose or modify the direction and magnitude of the vectors arising from the threads. In this way, they may affect the final aesthetic result.
When a thread (Thread cog 1 in Figure 1) is inserted, there are vector forces in both the upper and lower longitudinal plane of the thread. There are smaller vectors in the perpendicular plane all around the thread circumference throughout the length of the thread. In the case of Thread cog 1 (Figure 1), these perpendicular vectors are easily overpowered by the true ligaments, superiorly by the zygomatic-retaining ligament and inferiorly by the mandibular-retaining ligament. There is also influence, albeit small, from the nearby false ligaments, which, for practical purposes, can be ignored.
Perpendicular vectors
Perpendicular vector forces are of small magnitude and direction and aid to keep the thread in position. This is especially true in regard to Thread cog 1 (Figure 1), as, in most cases, the false masseteric ligaments may have been breached, thereby, for practical purposes, negating their influence. Therefore, it can be seen that the main vectors of clinical significance are the longitudinal vectors at both ends of Thread cog 1 (Figure 1), in line with the main body length of the thread.
In the case of Thread cog 1 (Figure 1), as previously stated, the inferior vector is all but cancelled by the mandibular-retaining ligament, especially in a medial direction from its periosteal attachment to the mandible.
With the distal smaller vectors, the resultant vector would be in the direction of the bi-section line of the longitudinal and perpendicular vectors. This is not a desirable vector, but, in clinical practice, it is not of significance, as it is weakened due to dissipation along the inferior border of the mandible.
The superior end of Thread cog 1 in Figure 2 has a vector (V1) that gives a force and direction in line with the longitudinal plane. This is a desirable vector.
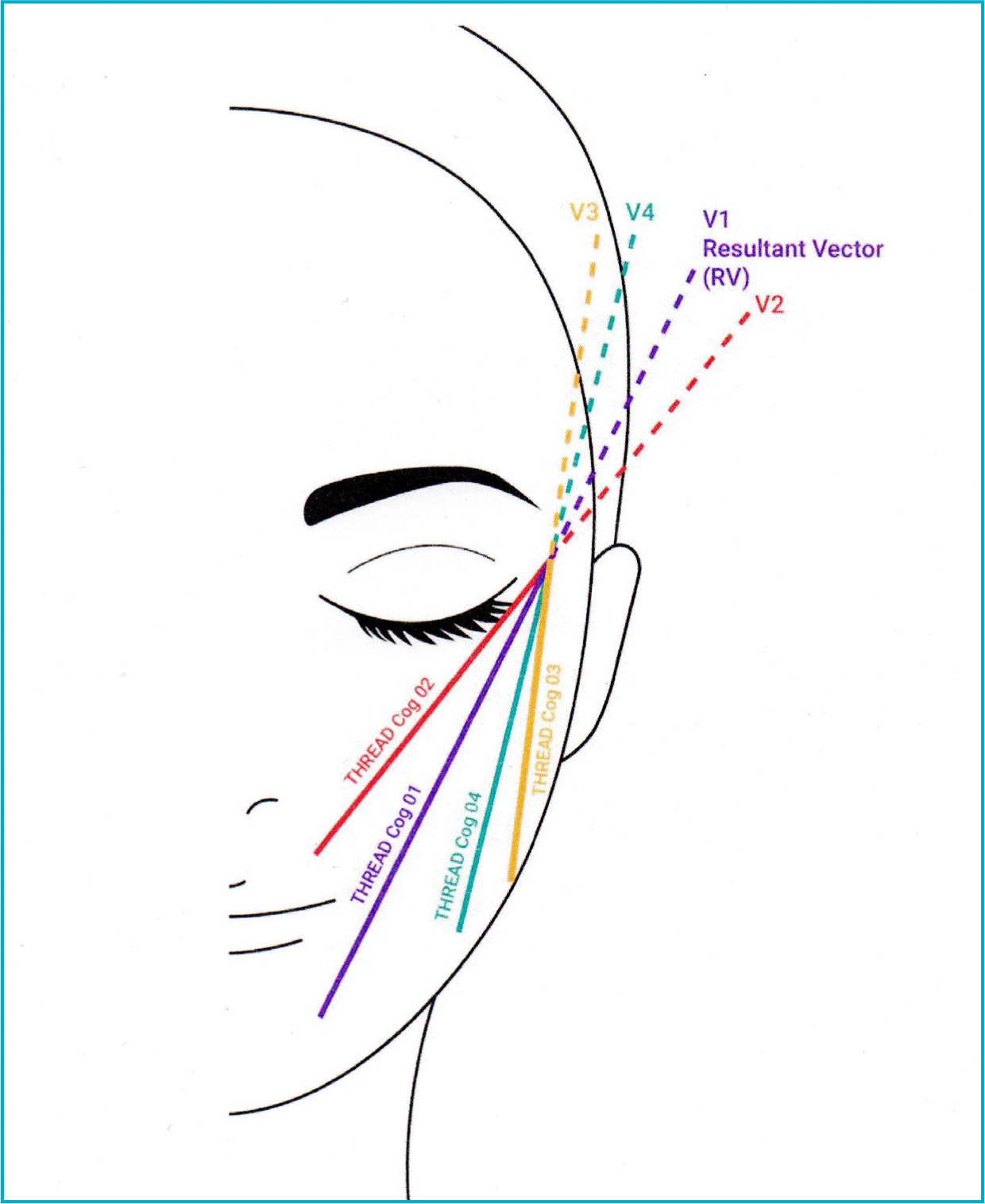 Figure 2. Vectors
Figure 2. Vectors
The porion is the point on the human skull that is located at the upper margin of each ear canal (external auditory meatus). It lies on the superior margin of the tragus. The vector forces from the pre-auricular ligament and the fibrous tissue condensation around the porion have little influence on the Thread cog 1 (Figure 1) vector in practice.
Shown in Figure 2, Thread cog 2 enters superiorly from the suprazygomatic margin, along the Frankfort plane, within 1.8 cm from the porion. The thread traverses towards the nasolabial fold, above the innominate fascia, breaching the false ligaments or, more accurately, the fibrous tissue condensation in the nasolabial fold area and some parts of the masseteric ligaments.
At this end, the thread has a vector force in the longitudinal plane of the thread and smaller vectors in the perpendicular plane. The longitudinal vector would create impingement of the upper lip and give an undesirable vector, giving a poor clinical result. In practice, this effect does not occur because the anatomy of the skin of the upper lip from the nasolabial fold is different from the cheek. Histological examination shows that the nasolabial fold superficial musculoaponeurotic system (SMAS) is a fibromuscular three-dimensional meshwork bolstered with fat cells (Langevin et al, 2011).
Minor vectors
The perpendicular thread ‘minor’ vectors are of small magnitude and direction and have little influence when opposed by the much stronger true zygomatic-retaining ligaments superiorly.
Inferior opposition comes from the false masseteric ligaments, but, in most cases, their effect is weak, as they may have been cut during thread insertion. The superior end of Thread cog 2 (Figure 2) has little opposition, as explained for Thread cog 1 (Figure 1). Thread cog 3 enters from the same entry point superiorly, and the end point is in the posterior jowl fat pad (Figure 2).
At the mandibular angle, the longitudinal and perpendicular vector forces are opposed by the platysma auricular ligament (a condensation of fibrous tissue where the lateral temporal-cheek fat compartment meets the postauricular fat compartment). Superiorly, there is little opposition, thereby giving rise to vector 3 (V3). Similar vectors apply to Thread cog 4, giving rise superiorly to vector 4 (V4) (Figure 2).
When all threads are in place, then the resultant vector is the in the direction of the average composite vectors between V1 and V4. This is the direction which is desirable to produce an upward facial tissue lift.
Cellular responses to thread placement
In addition to thread vectorisation, the clinical outcome is also dependent on many other factors involving the surrounding soft tissues, as previously stated. PDO thread placement creates a wound that disrupts the normal structure and function of these soft tissues. There is haemostasis, followed by an inflammatory reaction, which results in epithelialisation by fibrocytic cell conversion to fibroblast cells.
The insertion of the thread causes damage to the platelets, which release cytokines, interleukins and growth factors that start the wound healing process.
Collagen production
Fibroblast proliferation results in the production of ground substance, pro-collagen and collagen. Fibroblasts also differentiate from mesenchymal cells after 24 hours and reach maximal capacity after 10 days. This is the average timescale for tissue trauma. However, with thread placement, the thread is still in place after 10 days, so this effect is prolonged. This is part of the foreign body reaction, inducing fibroplasia in the tissues in which the thread is present. Due to the tension present, the fibroblasts undergo a morphological change and allow the tissues to accommodate to the tension present as a result of the placement of tissue-lifting threads.
Collagen production begins on the second day. At this stage, it is an amorphous gel. Maximum collagen production begins after 5 days, and wound healing is complete in 6 weeks. This is the neo-collagenic response to thread placement. Thread placement mainly prolongs the production of type 3 collagen (Neilson and Kendel, 2016).
The fibroblast produces collagen but also differentiates to myofibroblasts. These produce contractile proteins. Myofibroblasts are present after 5 days and have the ability to contract, similar to smooth muscle. They are eventually absorbed by apoptosis.
However, the placement of tissue-lifting threads causes the myofibroblasts to persist longer and are, therefore, helpful to the clinician, as they are synergistic to the facial displacement achieved by the threads due to their contractile ability. Clinically, they oppose skin laxity.
Prophylactic infection cover
It is important that bacteria are not introduced during thread placement, especially at the points of thread insertion.
Bacterial contamination results in the production of abnormal metalloproteases, which alter the balance of the inflammatory response and impair cytokine function. This affects the clinical outcome of the procedure and gives a poor result. A number of cases of post-operative infections have been seen after thread placement. It is now recommended that all cog placements, whether barbed or molded, should be done under prophylactic antibiotic cover (Otto et al, 2016).
Pressure garments
In clinical practice, facial lifting with threads is a painful procedure but well tolerated by most patients. It is operator skill-dependent, as well as technique-dependent.
The more skilled and experienced medical practitioner will be able to perform the thread-lifting procedure speedily, safely, with minimal pain and without error. This will reduce post-operative pain, as well the incidence of wound contamination, giving a good clinical result. Clinicians must go through a steep learning curve to achieve consistent good clinical outcomes.
As with all procedures, whether invasive or non-invasive, there is necessary downtime. In non-surgical thread procedures, clinical experience has shown that the patient wearing a facial pressure garment achieves many desired effects. These are as follows:
- The garment supports the face and prevents excessive movement during speaking and eating
- Gravity allows the tissues to drop, and this causes the cogs on the cog threads to impinge on the tissues, resulting in a degree of trauma and pain. The garment reduces this effect by maintaining compression
- The wearing of the garment aids the tissues in healing in the desired position
- Pressure garments worn during sleep for the first few days after thread placement hold the tissues in place and prevent tissue trauma from involuntary facial movements during sleep
- Many patients find the wearing of the garment aids recovery, and they feel that their recovery is more comfortable when asked at audit.
Conclusion
As can be seen, the practice of tissue displacement or face-lifting using threads is dependent on a variety of factors, which include the type of thread, its material composition, the patient's health and the clinician's skills, which will ultimately affect the final clinical result.
Clinicians should understand both macro and micro factors, which come into play during these procedures, and this article has tried to explain these. It is hoped that this goes some way in better understanding the factors involved, so that patients and their clinicians benefit, and better clinical outcomes are achieved.
Key points
- The presence of any pathological conditions that may need therapy or be a contraindication for any thread procedure
- The more skilled and experienced medical practitioner will be able to perfom the thread-lifting procedure safely, with minimal pain and without error.
CPD reflective questions
- What are the most clinically significant vectors?
- How can a pressure garment assist in the downtime process?



