
Despite the increasing use of polynucleotides, there exists a disparity in comprehensive regulatory guidelines, which raises concerns about standardisation and safety in clinical practice. This review calls for the establishment of robust, evidence-based regulatory standards that would ensure safe and effective application, aligning with international best practices.
To propel the field of aesthetic medicine forward, this study emphasises the necessity for continued research to validate the long-term efficacy and safety of polynucleotide treatments. It advocates for larger, randomised controlled trials to better understand the full scope of their therapeutic benefits and side effects. The integration of detailed mechanistic studies would also refine application protocols and enhance treatment outcomes.
Conclusively, while polynucleotides present a promising avenue for non-invasive rejuvenation therapies, their full integration into clinical practice demands a concerted effort to develop standardised guidelines and conduct comprehensive clinical evaluations. Such advancements will not only bolster the therapeutic repertoire of aesthetic medicine but also enhance patient safety and treatment efficacy, establishing a new standard in skincare treatment.
Chapter 1: introduction
Polynucleotide-based treatments are emerging as a promising approach in the field of aesthetic medicine, particularly for skin rejuvenation. This study aims to comprehensively evaluate the current knowledge on the safety, efficacy, and mechanisms of action of these treatments. By delving into the available literature and clinical data, the study seeks to shed light on how polynucleotide contribute to skin rejuvenation, identifying the primary mechanisms involved in their therapeutic effects.
Understanding the mechanisms by which polynucleotide promote skin rejuvenation is crucial for advancing their application in aesthetic treatments. These mechanisms may include cellular repair, stimulation of collagen production, and enhancement of skin elasticity and hydration. By elucidating these underlying processes, the study will provide a clearer picture of how polynucleotide-based treatments achieve their rejuvenating effects, paving the way for optimised therapeutic strategies.
Additionally, the study aims to evaluate the current UK guidelines for polynucleotide treatments in aesthetic medicine. By examining regulatory frameworks and clinical practice standards, it will assess the adequacy and effectiveness of existing guidelines in ensuring patient safety and treatment efficacy. This comprehensive evaluation will contribute to the development of informed, evidence-based recommendations for the use of polynucleotide treatments in skin rejuvenation, ultimately enhancing patient outcomes and advancing the field of aesthetic medicine.

1.1. Facial skin anatomy
The anatomy of the skin on the face, like that on other parts of the body, consists of three primary layers: the epidermis, the dermis, and the subcutaneous tissue (hypodermis).
Facial skin exhibits several distinct differences from the skin on the rest of the body, significantly influencing aesthetic treatment considerations. Structurally, facial skin is generally thinner, particularly around the eyes and lips, making it more susceptible to environmental damage and the visible signs of ageing, such as fine lines and wrinkles (Freedberg et al, 2003). The face also has a higher density of sebaceous glands, especially in the T-zone (forehead, nose and chin), leading to a greater propensity for oiliness and acne. This requires specialised treatments that can manage oil production without overly drying the skin (Drake et al, 2020).
The facial skin is more richly innervated and vascularised than other body regions, providing enhanced sensory perception but also making it prone to redness and irritation (Pessa and Rohrich, 2012). This vascularity requires careful consideration in treatments involving lasers, microneedling, or injections to avoid bruising and ensure even results. Additionally, the facial muscles are more active and expressive, contributing to dynamic wrinkles that necessitate targeted treatments like botulinum toxin to relax these muscles (Frost et al, 2004).
The face is continuously exposed to external factors such as UV radiation, pollution, and harsh weather conditions, necessitating robust sun protection and antioxidant-rich skincare regimens to mitigate damage (Heidemann and Kutz, 2010). Lastly, the aesthetic standards for facial skin are exceptionally high, with even minor imperfections being noticeable. This demands precision in aesthetic treatments, ensuring natural and harmonious results that enhance facial features while maintaining overall skin health. Thus, understanding these unique characteristics is crucial for developing effective, tailored aesthetic treatments for the face.
1.1.1. Dermal layers
1. Epidermis
The epidermis is the outermost layer of the skin. It provides a barrier to protect the body from environmental elements, pathogens, and dehydration.
2. Dermis
The dermis lies beneath the epidermis and is significantly thicker. It provides structural integrity and elasticity to the skin due to its fibrous and elastic tissue.
3. Subcutaneous tissue (hypodermis)
The hypodermis lies beneath the dermis and is composed mainly of adipose tissue (fat) and connective tissue. It serves as an insulator, shock absorber and energy reserve.
Specialised structures in facial skin
Regional variations
1.2. The history of polynucleotides
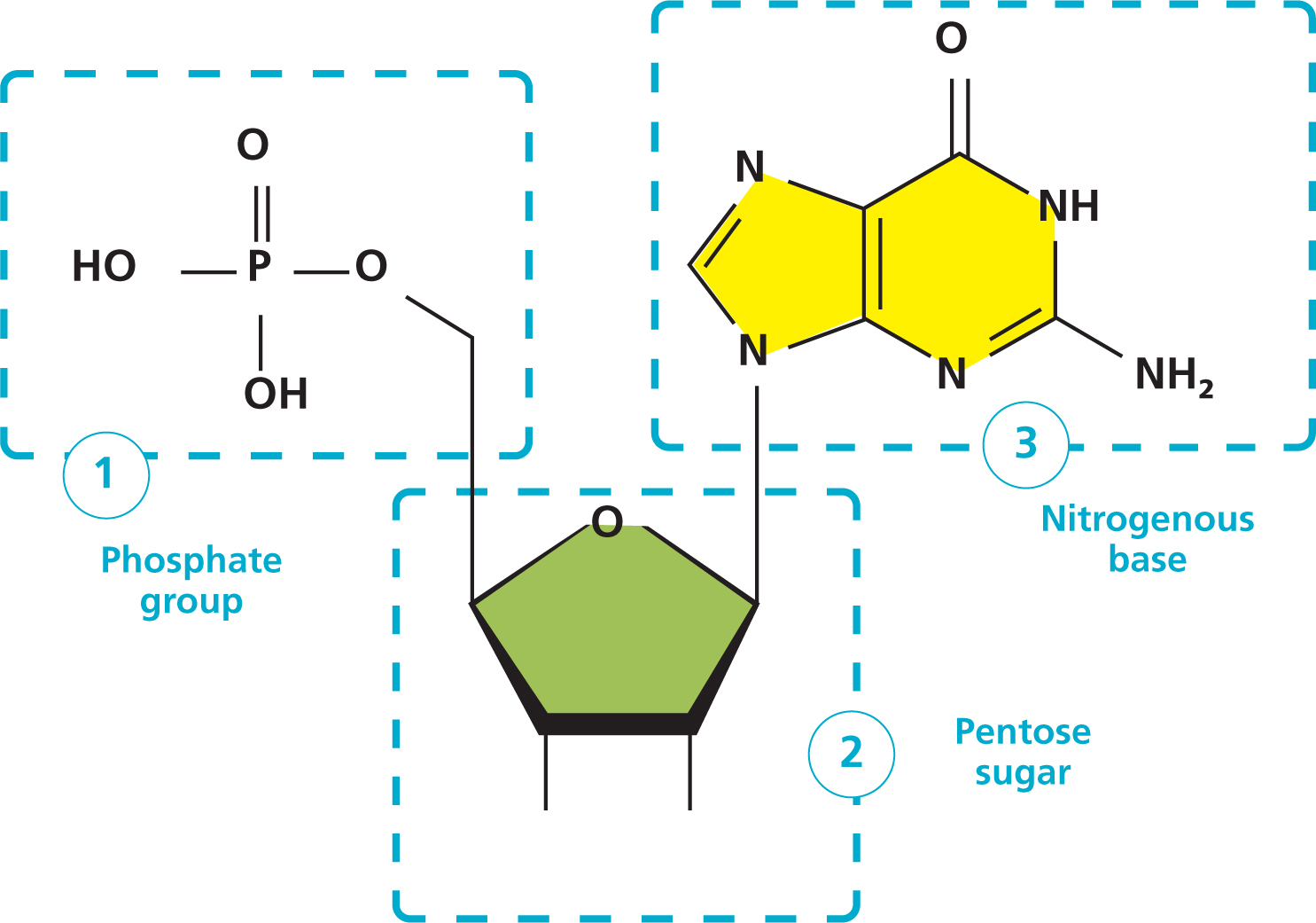
Polynucleotide, also known as nucleic acid polymers, have a rich history in the field of molecular biology and biotechnology. The study of nucleic acids dates back to the mid-1800s when scientists first began to explore the chemical composition and structure of DNA and RNA (Thomas, 1981).
In the realm of biological sciences, a profound revelation emerges through the intricate study of biological systems and the molecular structures of small molecules that influence them. By delving into the realm of biosynthetic pathways and other biochemical reactions, coupled with insightful analysis of polynucleotide sequences, a clearer comprehension of various biological enigmas has come to light. This synergy allows for the elucidation of phenomena that were once shrouded in ambiguity or obscurity.
In the mid-20th century, the discovery of the double helix structure of DNA by Watson and Crick in 1953 revolutionised our understanding of genetic material. This breakthrough laid the foundation for further research on nucleic acids and their role in cellular processes.
Polynucleotides have since been studied extensively for their diverse applications, ranging from genetic research and gene therapy to skincare and aesthetic medicine. In recent years, polynucleotides derived from sources like salmon DNA have gained attention for their potential benefits in skin rejuvenation and anti-ageing treatments. Overall, the history of polynucleotides is intertwined with key advancements in molecular biology and biotechnology, showcasing their significance in various scientific fields and applications (Kato et al, 1973).
It becomes evident that the significance of polynucleotide transcends conventional understanding and warrants a deeper appreciation for their multifaceted contributions to our comprehension of biological systems. This narrative underscores the indispensable nature of polynucleotide in shaping our insights into the complexities of life and calls for continued exploration and recognition of their pivotal role in the grand scheme of molecular biology and biochemistry.
The pivotal role of polynucleotide systems in unravelling fundamental aspects of life's genesis, the underpinnings of the genetic code, and the intricacies of protein biosynthesis mechanisms cannot be overstated. These intricate macromolecules not only harbour genetic information crucial for cellular processes but also orchestrate the translation of this information into functional proteins through the finely tuned ribosomal machinery.
1.2.1. Variation of polynucleotides and treatment areas
The pursuit of successful ageing has emerged as a focal point in preventive medicine, with aesthetic dermatology playing a significant role in meeting this objective. The utilisation of polynucleotide-based products presents a transformative approach that not only addresses volume loss but also enhances tissue regeneration, facilitating a more natural rejuvenation of skin health.
Polynucleotide are currently being utilised in various skin rejuvenation and anti-agieng treatments. In aesthetic medicine, polynucleotide-based formulations are known for their ability to stimulate collagen production, improve skin elasticity, and reduce the appearance of fine lines and wrinkles. Additionally, Polynucleotide offer antioxidant properties that help protect the skin from environmental damage and promote skin health. Their diverse applications in aesthetic dermatology highlight their role as a versatile and effective component in modern skincare regimens, catering to individuals seeking non-invasive yet impactful solutions for skin enhancement and rejuvenation (Oh et al, 2023).
Strong evidence includes the topical intradermal administration for peri-orbital rejuvenation. (Lee et al, 2020). In dermatology and aesthetic medicine, Polynucleotide-based products are commonly employed in procedures such as mesotherapy, skin boosters, and dermal fillers. These innovative formulations aim to improve skin texture, hydration, and elasticity while promoting tissue regeneration and reducing the visible signs of ageing. Polynucleotide have shown promising results in enhancing collagen production, increasing skin firmness, and minimising wrinkles and fine lines.
Moreover, emerging literature provides encouraging support for the anti-inflammatory properties of polynucleotide, particularly in addressing facial erythema. Research suggests that polynucleotide hold promise as effective agents for reducing facial redness and inflammation, potentially offering an alternative to conventional topical steroid treatments. The documented efficacy of polynucleotide in managing conditions such as facial erythema highlights their therapeutic potential in dermatological applications and underscores the shift towards innovative approaches for skin inflammation management (Lee et al, 2023).
Additionally, they are known for their antioxidant properties, which help protect the skin from environmental damage and promote overall skin health. The versatility and efficacy of polynucleotide make them a valuable component in contemporary skincare regimens, catering to individuals seeking non-invasive yet effective solutions for skin enhancement and rejuvenation. The process of skin ageing is influenced by both internal factors (intrinsic) and external factors (extrinsic), resulting in visible changes to the skin's structure and function. Intrinsic ageing is a natural part of getting older and involves programmed ageing processes within our cells due to factors like oxidative stress. Extrinsic ageing, on the other hand, is accelerated by external factors such as sun exposure and pollution, leading to the production of harmful compounds that can damage DNA and impair cell function (Shin et al, 2023).
As skin ages, the build-up of senescent (aged) cells and the breakdown of the skin's support structure contribute to the ageing appearance. To address signs of ageing, various skincare products and clinical procedures like chemical peels, injectables, and energy-based treatments have been developed. Each of these treatments targets different aspects of ageing. However, to create an effective anti-ageing plan, it's crucial to have a deep understanding of how skin ages. By grasping the fundamentals of how skin ages, researchers are encouraged to explore the world of anti-ageing treatments with a better understanding and appreciation of the underlying mechanisms (Lee et al, 2023).
A study involving a cohort of Korean women underwent multiple injections of long-chain polynucleotide intradermally at specified intervals to explore its efficacy in skin rejuvenation. The injections, administered in precise locations on one side of the cheek, led to marked improvements in pore size, skin thickness, skin tone, melanin levels, wrinkles and skin sagging, particularly notable in participants in their 30s and 40s. Importantly, the treatment exhibited a favourable safety profile with no reported serious adverse effects (Yi et al, 2022)
Polynucleotide are not only being used in skin rejuvenation but are also under investigation for their potential therapeutic applications in conditions such as osteoarthritis. In research studies, polynucleotide-based agents have shown promise in mitigating inflammation and cartilage degradation associated with osteoarthritis. By targeting specific pathways involved in joint damage and inflammation, polynucleotide offer a novel approach to potentially alleviate symptoms and slow down disease progression in osteoarthritis patients. This dual role of polynucleotide in both skincare and osteoarthritis underscores their versatility and expanding scope of application in diverse medical fields aimed at promoting tissue regeneration and overall wellbeing (Kuppa et al, 2023).

In summary, the intradermal injection of long-chain polynucleotide product emerges as a promising and secure modality for enhancing skin rejuvenation. The outcomes of this study suggest that this approach holds potential as an effective strategy in aesthetic dermatology for promoting skin health and combating the visible signs of ageing.
1.3. Clinical studies/trials
The research surrounding polynucleotides for skin rejuvenation exemplifies promising developments within aesthetic medicine, although it is still in a nascent stage. Initial clinical trials have underscored the beneficial impact of polynucleotides on enhancing skin attributes such as elasticity, hydration, and overall rejuvenation. Notably, these treatments have demonstrated potential for ameliorating fine lines, wrinkles, and atrophic scars. Despite these encouraging outcomes, the body of evidence requires cautious interpretation due to limitations in study designs, often characterised by small sample sizes and brief follow-up periods, which constrain the generalisability and long-term applicability of findings (Kim et al, 2020).
Furthermore, while research has started to unveil the mechanisms by which polynucleotide facilitate skin improvements—such as promoting cellular repair and boosting collagen production—these biological pathways warrant deeper investigation to optimise treatment protocols (Gomez et al, 2019). Although comparative studies have occasionally positioned polynucleotides as favourable or equivalent to established substances such as hyaluronic acid, these results must be replicated across broader and more diverse populations to validate efficacy and safety comprehensively.
Moreover, while the safety profile of polynucleotides appears favourable, with minimal reported adverse effects, the absence of extensive long-term safety data poses a challenge. Potential adverse effects, emerging from prolonged use or larger cohort studies, remain underexplored. This underscores the need for ongoing surveillance and extended-duration studies to ensure sustained safety.
The research trajectory has also been somewhat geographically and demographically limited, with most studies concentrated in specific regions and among homogenous population groups. The majority of clinical trials originate from South Korea. This geographical and demographic narrowness limits the wider applicability of the results, suggesting a pressing need for future research to encompass a variety of demographic profiles to ascertain how different skin types and genetic backgrounds respond to polynucleotide treatments.
The use of polynucleotide in cosmetics and aesthetic medicine can be traced back to advancements in various countries, but South Korea is particularly notable for pioneering the use of these compounds in skin rejuvenation treatments.
South Korea has been at the forefront of utilising polynucleotide in cosmetic and aesthetic medicine, with significant advancements beginning in the early 2000s. Initial research focused on the regenerative properties of polynucleotides, leading to clinical trials in the mid-2000s that demonstrated their efficacy in skin rejuvenation (Kim et al, 2008). By the early 2010s, polynucleotide treatments had gained widespread adoption in South Korean cosmetic clinics, bolstered by positive clinical outcomes and commercial success (Park and Lee, 2012). Further advancements in the late 2010s included improved formulations and the introduction of standardised training programmes for practitioners, ensuring consistent and safe application (Choi et al, 2018). South Korea's continuous research and innovation in polynucleotide treatments have cemented its global leadership in aesthetic medicine, influencing practices worldwide (Kim et al, 2021).
The study by Kim et al (2008) examines the effectiveness of polynucleotide treatments for skin rejuvenation, highlighting strengths and limitations. The randomised controlled trial design strengthens its credibility, demonstrating improvements in skin elasticity and hydration post-treatment. However, the unspecified sample size raises concerns about statistical power and generalisability. A short six-month follow-up period limits assessment of long-term safety and durability. Reliance on subjective measures like patient satisfaction introduces potential bias, necessitating inclusion of objective assessments. The study lacks discussion on underlying biological mechanisms of Polynucleotide effects, crucial for refining treatment protocols. Moreover, limited demographic diversity among participants restricts applicability across different skin types and ethnicities. Overall, while promising, the study underscores the need for larger, more diverse samples, longer-term follow-up, objective outcome measures, mechanistic insights, and broader demographic inclusivity to validate findings and guide clinical practices effectively.
More recently, a randomised, double-blind, split-face design of the study by Lee et al (2020) represents a robust methodological approach, ensuring a high level of internal validity and reducing bias in the evaluation of the effects of polynucleotide versus hyaluronic acid fillers for periocular rejuvenation. This design allows for a direct comparison of two treatments within the same individuals, controlling for between-subject variability and enhancing the reliability of the results. However, a critical aspect to consider is the sample size and demographic diversity of the participants, as these factors significantly influence the generalisability of the findings. This study had 27 participants, which would constitute a small sample size. Studies involving facial aesthetics must account for subjective evaluations of improvement, which can introduce bias despite blinding if not properly managed with validated assessment tools. Additionally, the duration of follow-up is crucial to assess the longevity of treatment effects; short follow-up periods may not adequately capture delayed adverse effects or the sustainability of the aesthetic improvements. Lastly, detailing the specific techniques and volumes of polynucleotides used is essential for reproducibility and clinical applicability, as variations in these parameters can affect outcomes. Overall, while the study design is strong, and is one of the most recent RCTs in polynucleotide there are limitations as outlined.
In summary, while polynucleotide hold significant potential for skin rejuvenation, the field requires more extensive and rigorous research to fully understand their capabilities and formulate evidence-based guidelines for their application in aesthetic medicine. As it stands, the initial efficacy and safety endorsements provided by current research offer a hopeful perspective, yet they also call for a tempered and critically informed approach to clinical application and further investigation.
1.4. Aims/hypothesis
Aims
The primary aim of this research project is to critically evaluate the existing literature on the efficacy of polynucleotide in skin rejuvenation, examining both the clinical outcomes and the underlying biological mechanisms. Additionally, this project aims to assess the current regulatory landscape and guidelines governing the use of polynucleotide in aesthetic medicine. This dual focus will provide a comprehensive overview of both the scientific validity and the regulatory framework of polynucleotide, offering insights into their potential benefits and limitations.
Objectives

By achieving these objectives, the research project will provide a robust analysis of the efficacy and safety of polynucleotide treatments in skin rejuvenation, alongside a critical evaluation of the regulatory environment. This comprehensive review will help clarify the standing of polynucleotides in aesthetic medicine in the UK and potentially guide future research and regulatory updates.

Chapter 2: materials and methods
2.1. Search strategy
Multiple databases were employed to source the literature for this review on polynucleotide and their effects on skin rejuvenation. Initially, a preliminary search was conducted using Google Scholar with the term ‘polynucleotide for skin rejuvenation’ to survey the available literature in this emerging field. In collaboration with the online library through the University of South Wales, this preliminary search helped to refine the search terms for the review to include more specific keywords such as “polynucleotide”, “skin rejuvenation”, “dermal repair”, “hydration” and “collagen synthesis”.
The final selection of articles was then conducted through PubMed, Medline and ScienceDirect using these refined keywords. Following this, the identified sources were briefly analysed to ensure alignment with the objectives of this review. The inclusion criteria were that the research questions of the articles must be directly relevant to the efficacy of Polynucleotide in skin rejuvenation, the studies must be primary research articles, and must have been published in peer-reviewed journals. Given the novelty and burgeoning interest in this field, no restrictions were placed on the publication date. Only studies published in English were considered, and no further limitations were imposed while searching PubMed and Scopus. The search strategy for ScienceDirect is detailed in Table 1.
A significant challenge encountered during the search was the limited number of trials and studies available on this specific topic. Additionally, the bibliographies of the included articles were scrutinised to identify any relevant studies that might have been overlooked in the initial database search.
2.2 Inclusion and exclusion criteria
The titles and abstracts of studies identified were independently screened for potential inclusion. Given the specificity of the topic—polynucleotide use in skin rejuvenation—the inclusion criteria were not overly restrictive. The review specifically targeted studies investigating the use of Polynucleotide in dermal rejuvenation, focusing on outcomes such as improved skin elasticity, moisture retention, and wrinkle reduction. Exclusion criteria were set to omit studies that employed Polynucleotide techniques but did not assess their effects on skin rejuvenation or studies that combined Polynucleotide treatment with other interventions, thus confounding the pure effects of Polynucleotide. Moreover, non-clinical trials such as opinion pieces, posters, news articles, or consensus reports were also excluded, as were studies investigating substances other than polynucleotides for skin rejuvenation.
This methodological approach ensures that the review is comprehensive and focused on relevant, high-quality scientific evidence, providing a clear and concise overview of the current state of research in the use of Polynucleotide for skin rejuvenation.
Chapter 3: results
In total, the chosen databases generated 80 studies; ScienceDirect: 61, Medline: 4, PubMed: 15.
From the 80 studies identified, 8 were excluded due to duplication, the author then excluded a further 45 articles after screening the titles and abstracts. Second, the remaining 35 articles were screened full text, and finally, of those, 14 articles were included in this review. Figure 1 shows the process of the search strategy.

The 14 articles that met the inclusion criteria, incorporating a variety of study designs and involving a total of 322 participants. These studies explored the effectiveness of polynucleotide monotherapy across skin rejuvenation for the face and neck.
The results highlighted a lack of detail in Polynucleotide sequencing, molecular targets, and dosage specifics, along with noticeable variations in source and production standards. Most studies showed a low risk of bias, indicating methodological soundness, yet there was a clear lack of detailed reporting on sequencing, targeted mechanisms, and molecular lengths. This review emphasises that polynucleotide research is still in its nascent stages and highlights the need for more rigorous studies to substantiate clinical outcomes.
Chapter 4: discussion
4.1 Risks and complications
Understanding the potential risks and side effects associated with skincare products containing polynucleotide is essential for safe and informed use. While these products hold promise for skin rejuvenation and health, it is crucial to consider the possible adverse outcomes that may arise from their application. Prior to incorporating polynucleotide into a skincare regimen, individuals should be aware of the associated risks to make informed choices about their skincare routine. By being knowledgeable about the potential risks and side effects, individuals can take necessary precautions, monitor their skin's response, and seek professional guidance if needed to mitigate any adverse reactions effectively. Some of the commonest risks and complications reported by Khan et al (2020) include:
4.2. United Kingdom guidelines for polynucleotides
In the UK, the regulatory framework governing the use of polynucleotide in aesthetic medicine is currently not well-defined. This gap is significant considering the increasing popularity and application of polynucleotide treatments for skin rejuvenation and related aesthetic procedures. The primary oversight bodies such as the MHRA and the GMC enforce general standards for safety, efficacy, and ethical practice within the broader cosmetic intervention sector, but specific guidelines targeting Polynucleotide treatments remain underdeveloped.

4.3. Mechanism of action in skin rejuvenation
Activation of the A2A receptor
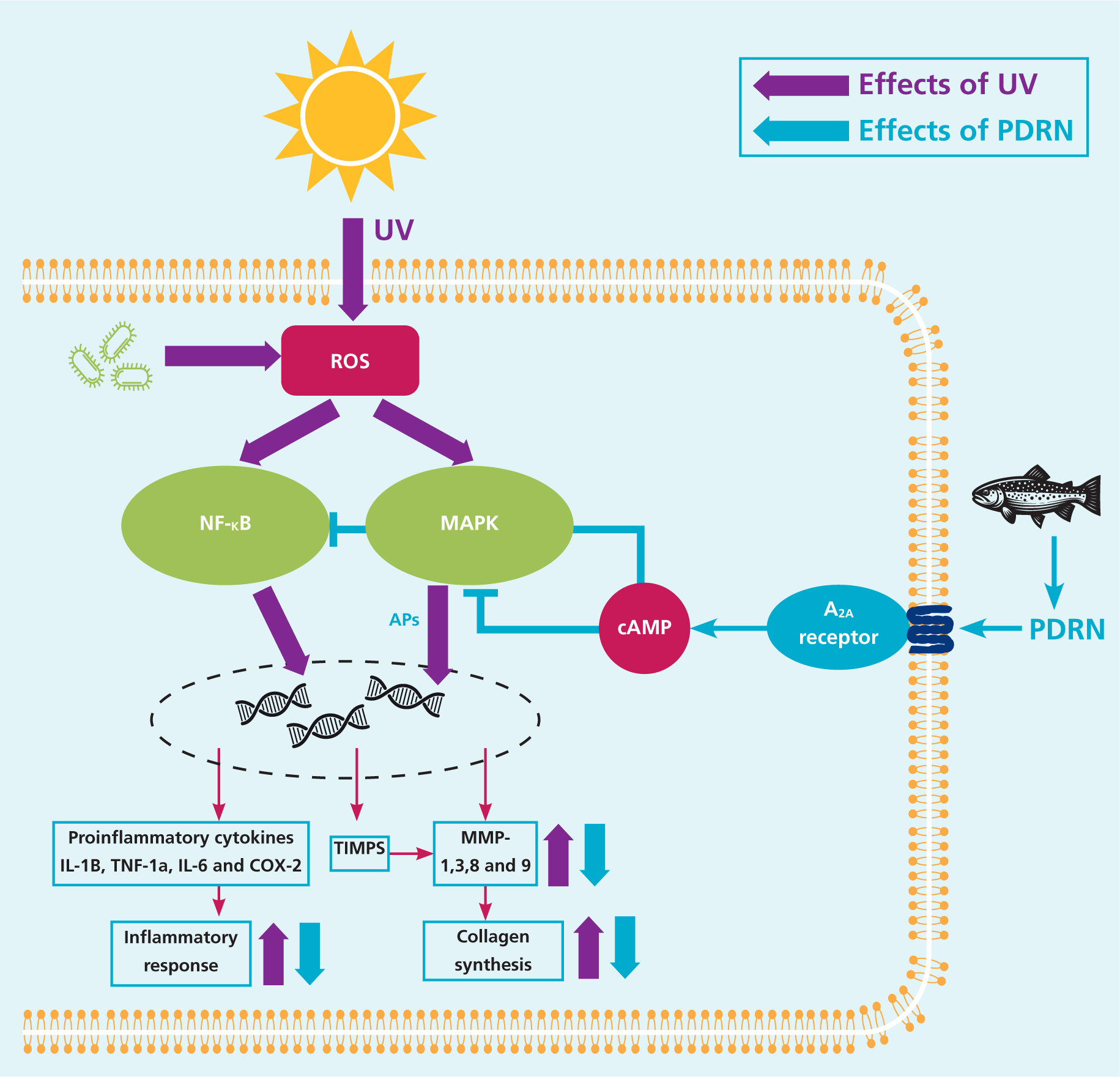
PDRN exerts its mechanism of action primarily through the activation of the adenosine A2A receptor. Adenosine receptors, particularly the A2A subtype, are identified as valuable targets for addressing disorders associated with ROS. When the A2A receptor is activated, it plays a pivotal role in regulating inflammatory responses, inhibiting apoptosis, and promoting tissue repair and healing processes (Ko et al, 2020).
According to Picciolo et al (2021) the activation of the A2A receptor leads to the modulation of the inflammatory response by inhibiting the NF-kB and MAPK signalling pathways, which ROS typically activates. This inhibition subsequently curtails the release of pro-inflammatory cytokines and stimulates the release of anti-inflammatory cytokines, contributing to a balanced inflammatory milieu.
The activation of the A2A receptor also results in an increase in cAMP concentration, which in turn inhibits the MAPK pathway. By inhibiting the MAPK pathway, PDRN effectively impedes the expression of MMP-1 and enhances collagen synthesis, promoting tissue regeneration and skin rejuvenation (Kim et al, 2020).
Overall, the action of PDRN in inhibiting the NF-kB and MAPK pathways showcases its ability to counteract the detrimental effects initiated by ROS, leading to a more controlled inflammatory response, enhanced tissue repair, and improved skin health.
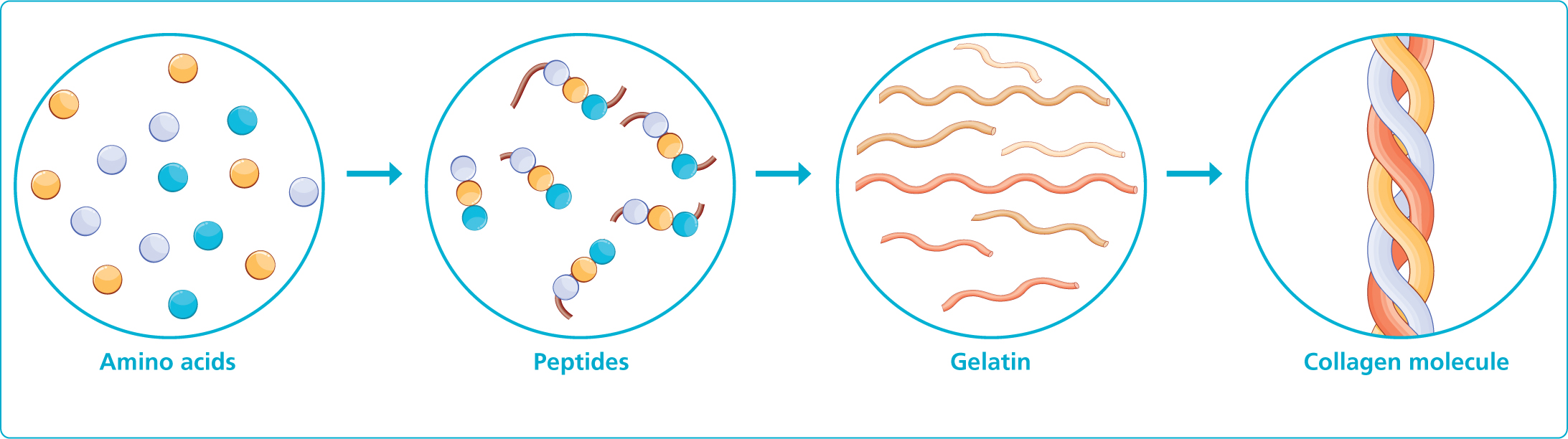
Collagen synthesis
Polynucleotide play a vital role in promoting collagen synthesis by enhancing the binding of adenosine to A2A receptors. Studies have shown that the application of polynucleotide in HDF led to a notable increase in collagen expression. This effect was dose-dependent, meaning that higher doses of polynucleotide resulted in greater collagen synthesis. In contrast, cells treated with hyaluronic acid did not exhibit the same level of collagen synthesis (Kim et al, 2020)
Further investigations using an adenosine A2A receptor agonist, CGS-21680, also demonstrated a significant dose-dependent enhancement of collagen production in treated cells. The pathway involved in this process involves Fli1, a key regulator of skin collagen levels, which inhibits collagen genes. Activation of the A2A receptor by the agonist CGS-21680 culminated in the reduction of Fli1 levels and an increase in CTGF expression and secretion. This leads to a subsequent rise in collagen production. Neutralising CTGF effectively prevented the increase in collagen synthesis, suggesting that the downregulation of Fli1 and upregulation of CTGF are pivotal steps in the collagen induction process following A2A receptor activation (Chan et al, 2013).
Concussively, the interaction between adenosine and A2A receptors triggers a chain of events that ultimately stimulates collagen synthesis. This process serves as a fundamental mechanism through which polynucleotide contribute to enhancing skin health and promoting tissue regeneration.
Anti-inflammatory effect
PDRN exhibits potent anti-inflammatory effects as demonstrated in various cellular and animal studies. When tested in murine macrophage and human chondrosarcoma cell lines, PDRN effectively attenuated inflammation induced by inflammatory stimuli like lipopolysaccharides and interleukin 1 beta (IL-1B). This anti-inflammatory response was attributed to PDRN's ability to inhibit the production of inflammatory cytokines, mediated by the activation of adenosine A2A receptors which regulate the cytokine network (Castelini et al, 2017).
Moreover, An et al (2017) reported that PDRN was found to boost the production of interleukin 10 (IL-10), an anti-inflammatory cytokine, while concurrently suppressing the release of nitric oxide and pro-inflammatory cytokines such as interleukin 12 (IL-12) and tumor necrosis factor alpha (TNF-a). Studies focusing on arthritic conditions and ischemic colitis models in animal subjects further reaffirmed PDRN's anti-inflammatory properties by showcasing reduced levels of inflammatory proteins like COX-2, IL-7, IL-1B, and TNF-a, as well as improved expression ratios of key regulatory molecules.
Similarly, in rodent models with lipopolysaccharides (LPS)-induced lung injury, PDRN treatment led to the downregulation of inflammatory mediators IL-6 and TNF-a, and a favourable shift in the expression balance of pro- and anti-apoptotic proteins. These collective findings underscore the promising anti-inflammatory potential of PDRN, positioning it as a valuable candidate for managing inflammatory conditions across various biological systems (Bitto et al, 2011).

Improving angiogenesis
Wellbrock and Arozarena (2015) reported that PDRN exerts remarkable tissue-repair capabilities, notably enhancing the skin healing process by significantly increasing the expression of VEGF, a crucial regulator of angiogenesis. The mechanism behind this enhancement involves PDRN stimulating VEGF production by activating the adenosine A2A receptor. This action results in elevated CD31, transglutaminase-II, and angioprotein levels, indicative of improved angiogenesis processes. The effectiveness of PDRN in promoting skin repair hinges on the activation of the adenosine A2A receptor, a fact corroborated by the reversal of its healing effects upon administration of DMPX, a selective adenosine A2A receptor blocker.
In experimental models simulating peripheral artery occlusive disease and thermal injuries, PDRN demonstrated its efficacy in promoting angiogenesis. In occlusive disease models, PDRN therapy induced an upsurge in VEGF expression, leading to enhanced blood flow restoration. Similarly, burn injury studies in mice illustrated accelerated burn wound healing and re-epithelialization following PDRN therapy, outcomes that were nullified in the presence of DMPX. In ischemic skin flap models, PDRN treatment was associated with increased blood flow and VEGF expression, underscoring its angiogenic properties (Bitto et al, 2008).
Collectively, these findings emphasise PDRN's role in facilitating angiogenesis, thus positioning it as a promising therapeutic agent for promoting tissue repair and angiogenesis in various pathophysiological conditions.
Anti-melanogenesis effect
PDRN offers a significant inhibitory effect on melanin synthesis in a dose-dependent manner, showcasing its potential in addressing skin hyperpigmentation. Studies have demonstrated that PDRN treatment results in a substantial decrease in intracellular tyrosinase activity in melanocytes, accompanied by reductions in MITF and TRP-1 levels. These factors play critical roles in melanin production within melanocytes, and their downregulation signifies PDRN's ability to modulate pigmentation processes effectively (Lee et al, 2016).

Further investigations revealed that PDRN directly hampers tyrosinase activity, leading to a notable reduction in cellular melanin content in melanocytes. This inhibitory effect extends to the suppression of key melanogenic proteins such as MITF, TRP-1, and TRP-2. Tyrosinase, which facilitates the conversion of tyrosine to dopaquinone, represents a pivotal enzyme in melanin synthesis, while MITF governs melanocyte function and melanin-producing gene expression (Noh et al, 2016). Similar studies also showcased PDRN's ability to inhibit melanogenesis in both Mel-Ab cells and human melanocyte-keratinocyte co-cultures, affirming its consistent anti-pigmentation effects. The modulation of melanogenic gene expression and the enzymatic activity of tyrosinase collectively contribute to PDRN's capacity to suppress melanin formation effectively (Khan et al, 2022).
In essence, by targeting key regulators of melanin synthesis and enzymatic processes involved in pigmentation, PDRN emerges as a promising agent for managing skin hyperpigmentation and promoting more even skin tone and complexion.
4.4. Contraindications
In recent years, polynucleotides have gained attention in the skincare industry for their potential benefits in skin rejuvenation and wound healing. These nucleotide-based compounds promote collagen production, improve skin texture, and enhance overall skin health. While initial studies (Khan et al, 2020) have shown promising results, it is essential to consider the contra-indications associated with using polynucleotides in skincare.
Understanding these boundaries can help individuals make informed decisions about incorporating polynucleotides into their skincare routine and manage their efficacy and safety expectations. Contraindications represent specific circumstances or conditions under which the use of polynucleotide may not be appropriate or advisable. These contraindications help individuals and healthcare providers identify situations where the risk of adverse effects or potential harm outweighs the potential benefits of using polynucleotide-based skincare products. By being well-informed about these contraindications, individuals can make informed decisions about incorporating polynucleotide into their skincare routine, thereby promoting skin health and minimising the risk of undesirable outcomes.
Incorporating polynucleotide into skincare is a relatively recent development that may present potential pitfalls and dangers due to the limited long-term data and a lack of comprehensive understanding of their effects. The novelty of polynucleotide skincare products raises concerns about unforeseen risks and adverse reactions that may have yet to be fully explored or documented (Kim et al, 2020).
With extensive research on polynucleotide long-term safety and efficacy, there is a degree of certainty regarding their interactions with various skin types, underlying conditions, or other skincare ingredients. The rapid emergence of polynucleotide-based skincare products also underscores the importance of ongoing monitoring, evaluation, and regulation to ensure consumer safety and to address any unforeseen complications that may arise with their use. Conducting thorough testing, clinical studies, and monitoring for potential side effects are essential to uncovering and mitigating any hidden dangers associated with using polynucleotide in skincare (Khan et al, 2022).
Cmmon contraindications reported by Khan et al (2020):
Furthermore, it is essential to conduct critical appraisals of scientific research when more robust evidence is available.
At present, some limitations of polynucleotide skincare products include:
Ultimately, empowering decisions by being aware of these limitations and considering them in the context of individual skincare needs and preferences, individuals can make informed decisions about incorporating polynucleotides into their skincare routine. Consulting with skincare professionals can provide personalised recommendations and guidance tailored to specific skin concerns and goals, further empowering informed decisions.
4.5. Other benefits
Several clinical studies have begun shedding light on the safety and efficacy of polynucleotides, offering encouraging findings to the medical community. Among these studies, a particularly notable one involving 40 patients sought to assess the outcomes of polynucleotide injections. Remarkably, no severe adverse effects were reported by any participants, and thorough physical examinations revealed no lingering skin abnormalities. The study further noted the absence of serious systemic adverse events, with both vital signs and laboratory data reassuringly in check throughout the study period. Importantly, a marked improvement in the condition of the participants was observed, aligning with the absence of any complications related to the injections (Kim and Chung, 2015).
In a separate study focused on diabetic foot ulcers, the positive impact of polynucleotide treatment was once again evident. Every patient showcased promising signs of improvement without encountering any associated complications, signifying the potential of polynucleotides in addressing such challenging medical conditions (Kim and Chung, 2015).
Moreover, another clinical investigation highlighted the favourable effects of polynucleotide on tissue oxygenation, inflammation, and angiogenesis post-treatment. This particular study underscored the multifaceted benefits that polynucleotide may offer in enhancing these essential physiological processes (Khan et al, 2022).
Additionally, a clinical trial emphasising the efficacy of Polynucleotide on skin grafts showcased promising results without any reported adverse effects. This further underscores the potential versatility and safety profile of Polynucleotide as a therapeutic intervention in various medical scenarios.
PDRN and the anti-ageing effects on skin:
Improvement of skin texture
As individuals age, collagen, the predominant protein in the body, undergoes structural alterations leading to the emergence of unwanted skin wrinkles, a visible hallmark of ageing. Collagen serves as a vital structural foundation in the human body, offering support to cells, tissues, and organs while playing a pivotal role in defining skin physiology through the creation of supportive networks within cellular structures (Cole et al, 2018).
Nevertheless, Ishi and Asuwa (2020) described various solutions that targeting skin enhancement which are available in today's market, encompassing treatments such as lasers, skin peeling, galvanic electricity, and oral supplements containing hydrolysate molecules. These diverse procedures share a common objective of stimulating collagen production to improve skin quality. Notably, treatment with PDRN has demonstrated efficacy in enhancing collagen synthesis. Recent research has delved into the augmentation of fibroblast collagen and elastin production by inhibiting MMP-1 activity; the resultant decrease in MMP activity has shown a concomitant increase in collagen synthesis.
MMPs play a critical role in elastin degradation, with elevated MMP levels linked to the degradation of Extracellular Matrix (ECM) components. Notably, PDRN has been observed to suppress MMP-1 and elastase expression, two key contributors to skin ageing and wrinkle formation. Elastase, a protease responsible for elastic fibre breakdown, has been associated with reduced skin elasticity when overexpressed. Ageing-related studies in mice have shown an age-associated increase in elastase activity, suggesting that inhibiting elastase activity could potentially mitigate the loss of skin elasticity. Additionally, MMP-1 also contributes to ECM breakdown, further emphasizing the importance of inhibiting MMP-1 through PDRN to support skin elasticity preservation. By targeting these key factors involved in skin ageing processes, PDRN emerges as a potential ally in combating the effects of ageing on skin elasticity and overall skin health (Khan et al, 2020).

DNA synthesis in skin rejuvenation
UV light-induced DNA damage is a key factor in skin ageing, leading to MMP-1 release and increased expression. PDRN inhibits MMP-1 and promotes angiogenesis and tissue regeneration by stimulating VEGF production via adenosine A2A receptor activation. PDRN provides nucleotides for salvage pathways, aiding in DNA synthesis and cellular regeneration, thus facilitating tissue healing and growth (Kim et al, 2014).
Hyperpigmentation prevention and treatment
Melanin overproduction from UV exposure or inflammation can lead to hyperpigmentation disorders. PDRN effectively inhibits melanin synthesis by suppressing melanogenesis, including reducing tyrosinase activity and MITF expression, promoting skin whitening. However, further research is needed to fully understand PDRN's mechanism of tyrosinase inhibition and its skin-whitening effects (Kim et al, 2020).
Hair regeneration
Pattern hair loss (PHL) is a common form of alopecia characterised by progressive hair thinning. Studies have shown that combining 1927-nm fractionated thulium laser with PDRN injections can significantly enhance hair thickness and count compared to PDRN alone. Additionally, combining PDRN with platelet-rich plasma (PRP) therapy has shown improvements in hair thickness, indicating enhanced hair health with PDRN treatment (Cho et al, 2016).
4.6. Limitations of the study
This study had several limitations. As the evolution of polynucleotide is still emerging within aesthetic medicine, the number of clinical trials is very small. The sample sizes in each study were also very small. The largest study had 143 participants (Cavallini and Papagni. 2007), while the smallest study had 5 (Park, et al, 2016). There is no standardisaed outcome measures and reported results ranged from skin hydration, fine lines, pigmentation, skin elasticity, scar improvement,
There is limited, quantifiable data, which fully illustrate the effect in these products. Although these agents are known to illicit inflammatory changes, more controlled studies are needed to better elucidate the biostimulatory capacity of such non-surgical treatments. (Fisher et al, 2024).
This study had several limitations, in aesthetic medicine, the study identified several significant challenges that underscore the emerging nature of this research area. A critical limitation noted in the review was the relatively small number of clinical trials focused specifically on polynucleotides, which poses substantial challenges to the robustness of the research framework within this field.
Among the studies examined, the largest encompassed 143 participants (Cavallini and Papagni, 2007), a sample size that, while the largest in this specific area of study, remains modest compared to the larger-scale trials typically required for more conclusive results in medical research. In stark contrast, the smallest study included only five participants (Park et al, 2016), illustrating the extreme variability in study sizes. Such small sample sizes severely limit the generalisability of findings and raise significant concerns about the reliability and applicability of the results to a broader context.
A notable issue highlighted in the review is the absence of standardised outcome measures across studies. The outcomes investigated varied considerably, encompassing skin hydration, fine lines, pigmentation, skin elasticity, and scar improvement. This lack of uniformity complicates attempts to synthesise data or perform comparative analyses across different studies. The absence of standardised outcome measures hinders the construction of a coherent narrative on the efficacy of polynucleotides, making it challenging to draw comprehensive conclusions from the existing literature.
Moreover, the review pointed out that much of the available data is qualitative and lacks the quantifiable metrics necessary for drawing clear, objective conclusions. While many studies suggest that polynucleotides trigger beneficial inflammatory responses, the precise biostimulatory capabilities of these treatments remain poorly elucidated. As noted in Fisher et al (2024), there is a pressing need for more controlled studies to better understand these mechanisms.
Nevertheless, across all reviewed studies, no significant adverse effects were reported from the treatment protocols, underscoring the outstanding safety profile of this innovative approach (Cavallini et al, 2021). This distinct attribute differentiates it from other conventional aesthetic treatments that achieve comparable outcomes but often carry a higher risk of side effects. This favourable safety record not only enhances the appeal of polynucleotide therapies within the realm of aesthetic medicine but also reinforces their potential as a preferable alternative for patients seeking minimally invasive options to treat skin ageing and preventative ageing.
The author of the review emphasised the necessity for future research in aesthetic medicine, particularly non-surgical interventions involving polynucleotides, to adopt more rigorous methodologies. This includes implementing larger, more diverse participant groups, employing standardised protocols for measuring outcomes, and extending follow-up periods to assess long-term effects. Such advancements are crucial for the field to progress and for the integration of polynucleotide therapies into clinical practice to be based on solid scientific evidence.
While the field of polynucleotides in aesthetic medicine holds considerable potential, it is currently limited by significant research shortcomings. The study concludes that there is a compelling need for future investigations to utilise more robust study designs and standardised measurement tools to advance understanding and clinical application of polynucleotide therapies effectively.
4.7. Recommendations
Based on a comprehensive literature review on the efficacy of polynucleotides in skin rejuvenation and the examination of the regulatory status and guidelines around polynucleotides, several recommendations can be made to enhance the practical application, research, regulatory oversight, and clinical outcomes associated with these treatments:
Recommendations for clinical practice:
Recommendations for research:
Recommendations for regulation:
Recommendations for policy development:
These recommendations aim to support the integration of polynucleotide treatments into clinical practice safely and effectively while ensuring robust scientific backing and regulatory oversight. By addressing these key areas, the field of aesthetic medicine can continue to advance in a manner that prioritises patient outcomes and safety.
Chapter 5: conclusion
In this comprehensive literature review, we have evaluated the efficacy of polynucleotides in skin rejuvenation alongside the regulatory status and guidelines governing their use within aesthetic medicine. Polynucleotide treatments have shown promising potential in improving skin hydration, elasticity, and overall dermal health due to their influence on cellular repair and collagen production (Lee et al, 2020). These findings suggest a significant capability for polynucleotides to mitigate the effects of ageing, such as fine lines and wrinkles, thereby enhancing skin appearance and texture.
Despite these benefits, the regulatory framework for Polynucleotide remains underdeveloped, which may hinder their broader adoption and standardisation in clinical practice. The existing literature reveals stark variations in study designs and a prevalence of small sample sizes, which limits the generalisability of results and underscores the need for further large-scale, rigorous studies (Gomez et al, 2019). This gap in research highlights the emerging nature of polynucleotide treatments within the field and points to the necessity for a more structured research agenda to establish robust, evidence-based practices.
Moreover, the efficacy of polynucleotide, while notable, necessitates a cautious interpretation due to the nascent stage of most studies. Current research has begun to explore the mechanisms underlying their rejuvenating effects, yet more detailed studies are needed to fully understand and optimise these complex biological processes (Smith and Zhao, 2018). Furthermore, the clinical outcomes associated with polynucleotide treatments must be evaluated over longer periods to fully ascertain their long-term safety and effectiveness (Chen et al, 2022).
Reflecting on the regulatory landscape, there is a pressing need for specific guidelines that address the use of Polynucleotide in aesthetic medicine. Such guidelines would ensure patient safety and uphold high standards of treatment efficacy. The United Kingdom, in particular, could benefit from examining established protocols in countries like South Korea, where polynucleotide treatments have gained significant traction and are supported by a more definitive regulatory framework (Kim et al, 2021).
In conclusion, while the initial findings regarding Polynucleotide are promising, the aesthetic medicine community must push for more comprehensive studies and a clearer regulatory approach. This will help substantiate the safety profile of polynucleotides and define standardised treatment protocols, ultimately enhancing patient outcomes in skin rejuvenation therapies. Through a concerted effort in research, regulation, and practice, polynucleotide can potentially become a cornerstone treatment option in the ever-evolving field of aesthetic medicine.



