

Considered by many as the gold standard of anti-ageing ingredients, the use of retinoids in topical cosmetics products has become increasingly popular with both healthcare professionals and patients. This can be partly attributed to their effectiveness in regulating epithelial growth and differentiation that maintains the structural and functional integrity of the skin (Zasada and Budzisz, 2019).
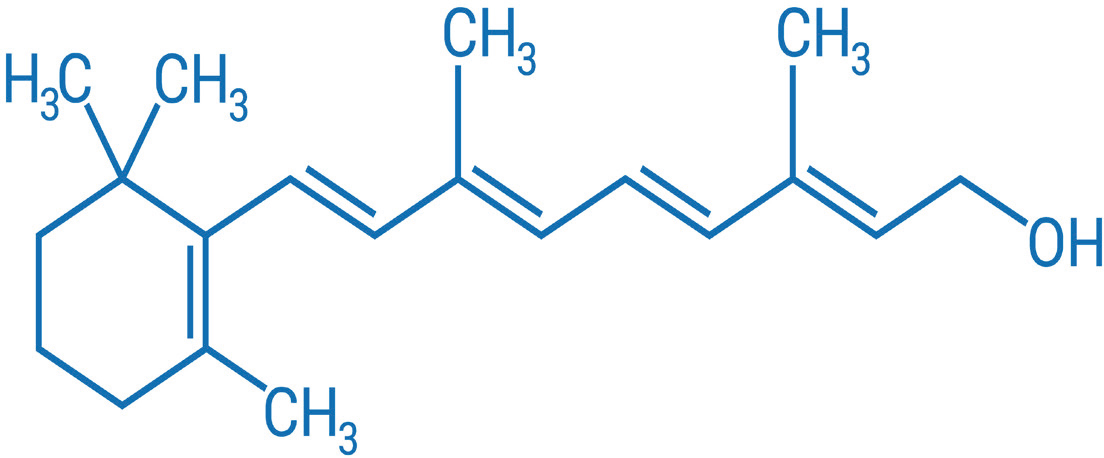
Retinoids are compounds of natural, biologically active forms of vitamin A (including retinol, retinal, and retinoic acid) (Motamedi et al, 2022) as well as synthetic analogues of adapalene (Babamiri and Nassab, 2010). They were first used to treat dermatologic conditions in the early 1970s, the discovery of which is attributed to Dr. Albert Kligman and colleagues who explored the use of tretinoin (retinoic acid) for treating acne (Kligman et al, 1984).
The discovery led to the evolution and broader application of retinoids in dermatology being used to treat multiple other dermatological indications including pigmentation and ageing, with tretinoin (retin-A) becoming the first topical retinoid to be FDA approved to treat acne in 1971 (Baldwin et al, 2013).
As retinoids are lipophilic molecules, they exert their effect by their ability to diffuse through cellular membranes. Once they are inside the cells, they bind to specific nuclear receptors and modulate the expression of the genes involved in cellular proliferation and differentiation.
Retinoids naturally occur in the skin, with retinol and retinyl esters being the most abundant form. Conversion of retinol to the active form involves oxidation to retinaldehyde, which is then oxidised to form the active tretinoin.
Retinoid popularity shows little signs of abating, as the global retinoid market size is estimated to increase from $1.63 billion USD to $3.05 billion USD and is expected to grow at a compound annual growth rate (CAGR) of 6.5% from 2024-2034 (Future Market Insights, 2024).
Regulatory changes
Retinoids have recently come under scrutiny due to recent changes in European Union (EU) cosmetics regulations where the Scientific Committee for Consumer Safety (SCCS) concluded that ‘overall consumer exposure, although low, may be of concern for consumers with the highest exposure to vitamin A (5 % of the total population) from food and food supplements’ (European Union Commission Regulation, 2024).
Therefore, from November 1 2025, retinol, retinyl acetate and retinyl palmitate will face restrictions in concentrations, with new levels set at 0.3% for face products (previously at 1%) and 0.05% for body products (European Union Commission Regulation, 2024).
Whilst these regulations only concern the EU, their influence is likely to be felt on a global scale, as brands are unlikely to invest significant resources in creating market-specific formulations. Therefore, it is likely that brands will sell their EU compliant formulations across all markets.
The four generations of retinoids
Although retinoids as a class have similar mechanisms, based on their unique molecular structures and properties, retinoids can be divided into four generations (Motamedi et al, 2022):
1) First generation (natural retinoids)
Monoaromatic compounds obtained by modifying polar groups at the end and side chain of the polyene vitamin that does not act selectively — retinol and its metabolites — retinal, tretinoin, isotretinoin. Retinol, retinal, and retinoic acid have the same biological features as vitamin A.
2) Second generation (monoaromatic retinoids)
Synthetic compounds in which the cyclohexene ring is replaced by a benzene ring; synthetic analogues of vitamin A (etretinate, acitretin both oral).
3) Third generation (polyaromatic retinoids)
Formed as a result of cyclization of polyene side chain and characterised by selective activity towards receptor (arotinoid, adapalene, tazarotene).
4) Fourth generation
Like trifarotene which is RAR-y selective retinoid and this helps with side effects.


Retinoid benefits
Ageing
Vitamin A and its derivatives are among the most effective substances at slowing the ageing process (Zasada and Budzisz, 2019). Anti-wrinkle properties of retinoids promote keratinocytes proliferation (Arto Määttä et al, 2023), strengthen the protective function of the epidermis (Quan, 2023), reduce transepidermal water loss (TEWL) (Arto Määttä et al, 2023), protect collagen against degradation and inhibit the activity of metalloproteinases which is the enzymes that can break down proteins, such as collagen (Sorg et al, 2005; Sorg and Saurat, 2014). Retinoid activity is related to high affinity for nuclear receptors: RAR – retinoid acid receptors and RXR — retinoid X receptors (Zasada and Budzisz, 2019; Sharma et al, 2022).
Pigmentation
Retinoids reduce pigmentation on skin and contribute to a proper distribution of melanin in the skin (Griffiths et al, 2023; Milosheska and Roškar, 2022). Topically applied retinoids also influence the function of melanocytes, providing regular arrangement of melanin in the epidermis (Aubert et al, 2018; Ortonne, 2006; Zasada and Budzisz). They also block the transport of melanin to epidermal cells and reduce the activity of stimulated melanocytes (Motamedi et al, 2022).
Acne
Due to retinoids exerting anti-comedogenic effects, they regulate the process of shedding within sebaceous glands ducts. Retinoids also decrease the activity of enzymes participating in lipogenesis and block differentiation and cellular divisions of sebocytes (Kajal and Nassab, 2010; Dreno et al, 2022; Del Rosso, 2022). Retinoids currently approved by the US FDA for the treatment of acne are as follows: tretinoin (7 gel doses [0.01% to 0.1%], 3 cream doses [0.025% to 0.1%], 0.05% lotion); adapalene (0.1% solution, 0.1%, and 0.3% gel, 0.1% cream, 0.1% lotion); tazarotene (0.1% gel, 0.1% cream, 0.1% foam, 0.045% lotion); and trifarotene (0.005% cream) (Ogé et al, 2019). These retinoids can be used as monotherapy or in combination with other non-retinoid treatments.
Retinoid types
Retinol
Retinol is the alcohol form of vitamin A (Lumen Learning, 2024) and may be more irritating if the skin has not been acclimatised or has limited numbers of vitamin A receptors in the cell membrane. Fat soluble retinol penetrates the stratum corneum and slightly penetrates the dermis (Zasada and Budzisz, 2019). When retinol reaches a keratinocyte, it enters its interior and binds to an appropriate receptor. There are four groups of receptors with high affinity towards retinol (CRBP). Retinol stimulates the cellular activity of keratinocytes, fibroblasts, melanocytes and Langerhans cells (Zasada and Budzisz, 2019). Retinol reduces oxidative stress and lipid peroxidation that can cause premature ageing (Papaccio et al, 2022). Retinol, by interacting with receptors inside keratinocytes, accelerates their proliferation, strengthens the epidermal protective function, reduces transepidermal water loss, stimulates fibroblasts to synthesise collagen fibres and protect against their degradation and improves skin elasticity by removing degenerated elastin fibres. Retinol also inhibits the activity of metalloproteinases, which are responsible for the degradation of the extracellular matrix, enhances remodelling of reticular fibres, promotes angiogenesis in the papillary layer of the dermis, re-activates vitamin A receptors found in skin cells and restores cellular homeostasis (Zasada and Budzisz, 2019).
In vitro, retinol has been shown to be 20 times less potent than retinoic acid (Spearings, 2021).
Currently, all cosmeceutical products with retinol do not require prescription. As a result, 3–6% retinol can be found in peels for potent acne, ageing or pigmentation treatment. Retinol is actively used as a combination treatment with antibiotics like clindamycin phosphate, which would need a prescription from a doctor. An adaptation period should be recommended for clients on retinol such as: twice a week for two weeks, every other day for the following two weeks. If the skin can tolerate the ingredient, it can be increased to daily use. If there is any sensitivity, reduce the frequency.
Retinoic acid (tretinoin)
Tretinoin, also known as all-trans-retinoic acid (ATRA), is a naturally occurring derivative of vitamin A (retinol) and it is a first-generation retinoid. Retinoic acid stimulates the process of epidermal cell proliferation, accelerates the elimination of sebum remaining in ducts, therefore reducing inflammation in sebaceous glands; loosens connections among cells in stratum corneum and inhibits keratosis (Zasada and Budzisz, 2019). Together with adapalene, it is the most effective retinoid for the treatment of acne, surpassing the benefits of retinaldehyde and retinol, which are more suited to be used for the improvement of wrinkles (Thielitz et al, 2005). Retinoic acid is a prescribed retinoid that can also be used to improve fine wrinkling, mottled hyperpigmentation, roughness associated with photodamage (Boswell, 2006; Burlengo-Ransby et al, 1993; Callendar et al, 2022).
Although the exact mechanism of action of RA is unknown, current evidence suggests that the effectiveness of RA in acne is due primarily to its ability to modify abnormal follicular keratinisation. Comedones form in follicles with an excess of keratinised epithelial cells. RA promotes the detachment of cornified cells and the enhanced shedding of corneocytes from the follicle. By increasing the mitotic activity of foaaaallicular epithelia, RA also increases the turnover rate of thin, loosely adherent corneocytes. Through these actions, the comedo contents are extruded and the formation of the microcomedone, the precursor lesion of acne vulgaris, is reduced. RA also causes dispersion of melanin granules (Thielitz et al, 2008). The side effects of topically applied high concentrations of RA can include redness, irritation, and flaking, and while impressive results have been achieved, client compliance is usually low, with expectations not always met. An adaptation period should be recommended for clients on retinol such as twice a week for two weeks and every other day for the following two weeks. If the skin can tolerate the ingredient, it can be increased to daily use. If there is any sensitivity, reduce the frequency (Yasinski, 2024; Szymański et al, 2020).


Retinalaldehyde (retinal)
Retinalaldehyde (retinal) is a first-generation topical retinoid used in skin lightening, skin depigmenting, skin rejuvenation, anti-ageing, and anti-glycation products.
Retinal is synthetically produced from B-carotene. However, it can also be directly oxidised from retinol. Retinal can be reversibly reduced to produce retinol or it can be irreversibly oxidised to produce retinoic acid (Kedishvili, 2016).
Retinoic acid is produced in two sequential oxidative steps. First, retinol is oxidised reversibly to retinaldehyde, and then retinaldehyde is oxidised irreversibly to retinoic acid, by retinaldehyde dehydrogenases (e.g., RALDH2) or some enzymes of the CYP family and then stimulates the epidermal cell proliferation. The best described active retinoid metabolites are 11-cis-retinal and the all-trans and 9-cis-isomers of retinoic acid (Lavudi et al, 2023).
Retinal inhibits collagenase, which is an enzyme that breaks down collagen. Retinal compounds are highly reactive, especially with alcohols and amines, and this may explain their antibacterial action, which is independent of nuclear receptors (Lay et al, 2024).
Adapalene (ADP)
Adapalene is a third-generation topical retinoid used for the treatment and/or maintenance of mild to severe acne (acne vulgaris). Adapalene has comparable efficacy, but a superior safety profile as opposed to tretinoin. Extensive alteration of the retinoic acid molecular frame has resulted in the evolution of adapalene, a more durable, less irritating compound with receptor selectivity (Cunliffe et al, 1997; Thiyboutot et al, 2006; Langer et al, 2007; Korkut and Piskin, 2014). One meta-analysis used 900 patients compared 0.1% adapalene and 0.025% tretinoin gel to treat acne patients. This showed that adapalene demonstrated equivalent efficacy to tretinoin in terms of reducing total lesion count. Additionally, adapalene demonstrated a more rapid efficacy, as evidenced by a significant difference in the reduction of inflammatory and total lesions at week one. It also demonstrated considerably greater local tolerability.
Adapalene is anti-comedogenic (Cunliffe et al, 1998), inhibiting the formation of further comedones and inflammatory lesions, and works to decrease inflammation by changing the innate immune response (Yehia et al,2024). Like similar retinoid compounds, adapalene is chemically stable and shows remarkable photostability (Rusu et al, 2020). Adapalene has the unusual ability to restrain keratinocyte differentiation and reduce keratin deposition. This feature makes adapalene an effective treatment for keratosis pilaris as well (Bruno, 1993).
Adapalene is extremely lipophilic (Shroot et al, 1997). When applied topically, it quickly penetrates hair follicles (Rolewski, 2003), and penetration occurs 5 minutes following topical application (Rusu et al, 2020). After infiltration into the follicle, adapalene binds to nuclear retinoic acid receptors (RAR)-beta and RAR-gamma (mainly); this complex afterward binds to one of three retinoid X receptors (RXRs), which as a complex can bind DNA to modulate transcriptional activity. Adapalene has been shown to hinder HeLa cell proliferation and human keratinocyte differentiation (Toleymat et al, 2023). These results primarily account for adapalene's comedolytic and noncomedogenic properties.
In addition, adapalene changes the immune response by down-regulating toll-like receptor 2 (TLR2) expression and hindering the transcription factor activator protein 1 (AP-1). TLR-2 recognises cutibacterium acnes (formerly propionibacterium acnes), the bacterium principally linked with acne. TLR-2 activation causes nuclear translocation of AP-1 and downstream proinflammatory gene regulation. Hence, adapalene has a general anti-inflammatory effect, which diminishes inflammation-mediated acne symptoms (Rusu et al, 2020). These complexes then bind to the retinoid X receptor which induces gene transcription by binding to specific DNA sites, thus modulating downstream keratinocyte proliferation and differentiation. This results in the normalisation of keratinocyte differentiation, allowing for decreased micro-comedone formation, decreased clogging of pores, and increased exfoliation by increasing cell turnover. Adapalene is also regarded as an anti-inflammatory agent, as it suppresses the inflammatory response stimulated by the presence of cutibacterium acnes and inhibits both lipoxygenase activity and the oxidative metabolism of arachidonic acid into prostaglandins (Shroot et al, 1997),
Retinyl palmitate
Retinyl palmitate is the ester of retinol and palmitic acid. As well as being the most abundant form of vitamin A storage in animals, it is also one of the most used vitamin A derivatives in the skincare industry. It is used in different types of skincare products (primarily rejuvenating, nourishing and after-sun products), and is ideal for the advanced treatment of pre-conditioned skin.

There is no significant evidence in the literature to support the effectiveness of topical retinyl-acetate and retinyl-palmitate as anti-aging agents. Topical retinyl palmitate, however, has been shown in animal and human studies to offer some degree of UV protection by an antioxidant mechanism (Piskin and Uzunali, 2007).
The esters of vitamin A play a pivotal role in cell metabolism and homeostasis. Vitamin A cellular receptors numbers are increased by the topical application of retinyl palmitate. Retinyl palmitate is converted into retinol as it passes through the cell membrane, where it is converted to retinoic acid within the cell, increasing DNA activity. Oil solubility makes this ester ideal for the treatment of oxidative stress and lipid peroxidation. It re-activates vitamin A receptors found in skin cells and restores cellular homeostasis (O'Byrne and Blaner, 2013; Kajal and Nassab, 2010).
Importance of effective skincare science education and personalised consultations
Robust skincare knowledge and advanced ingredient knowledge are all key to recommending safe and effective skincare regimens that contribute to optimal patient outcomes. It forms the basis of the patient's consultation, encourages integrity and ensures that any information given to patients is factually sound, clinically proven, and scientifically based. It also offers practitioners a greater depth of understanding of the product formula, and to match the product ingredient list to the function, quality, and effectiveness of the product. It also ensures that the recommended treatment plan is personalised to the unique needs of the patient.
The importance of tailoring your patient's treatment plan should not be underestimated. Each client's skin is unique and should be treated as such. Factors such as skin type, previous use of retinoids, and individual skin concerns should guide a practitioner's recommendations.
Additionally, understanding the percentage of active ingredients is critical to successful outcomes, especially when recommending actives like retinoids. Understanding the appropriate potency can make a significant difference in the efficacy and tolerability of these products.
When it comes to retinoids, finding a balance between effectiveness and client tolerability is key. This is because high percentages of retinoids can lead to irritation, dryness, and peeling, particularly for clients new to retinoids or who have sensitive skin. It is crucial to choose a soothing formulation and perhaps begin with an encapsulated retinoid that the skin can tolerate daily. There is a tendency to start with a higher percentage, but starting with a lower retinoid percentage can prove more effective. This is because it allows the skin to gradually acclimate and allows the retinoid to be used daily without causing significant irritation. Once the skin's tolerability is tested, the concentration can be increased if necessary.
Conclusion
Retinoids remain a popular and effective choice of topical treatments for patients and healthcare professionals when treating indications such as acne vulgaris, pigmentation, and issues related to ageing. Healthcare professionals should ensure that the skin's tolerability to retinoids is assessed and personalised to the unique needs of the patient. Consideration and caution should be taken pertaining to contradictions, and new regulations adhered to once they come into effect.
Key points
- Retinoids are compounds of natural, biologically active forms of vitamin A (including retinol, retinal, and retinoic acid) as well as synthetic analogues of adapalene
- Retinoids are a multi-faceted ingredient group and can be used to treat several indications including skin ageing, acne and hyperpigmentation
- Understanding retinoid potency is critical to successful outcomes and can make a significant difference in the efficacy and tolerability of topical products. Therefore, you should ensure a full and through educationbased consultation with the client has taken place prior to devising a treatment plan
- New EU regulations will come into force from November 1 2025, stipulating that, retinol, retinyl acetate and retinyl palmitate will face restrictions in concentrations, with new levels set at 0.3% for face products (previously at 1%) and 0.05% for body products (European Union Commission Regulation, 2024).
CPD reflective questions
- Are you familiar with the different types of retinoids? Are you aware of what indications retinoids can treat?
- Are you able to differentiate between the various types of retinoids when creating personalised treatment plans for patients?
- How do you approach patient education regarding the use of retinoids, particularly in addressing common misconceptions and ensuring compliance?
- Are you aware of the potential benefits and risks associated with the use of retinoids in long-term skincare regimens?



